 |
 |
| Tuberc Respir Dis > Volume 77(4); 2014 > Article |
|
Abstract
Background
In Korea, patients with destroyed lung due to tuberculosis (TB) account for a significant portion of those affected by chronic pulmonary function impairment. The objective of our research was to evaluate the efficacy of inhaled tiotropium bromide in TB destroyed lung.
Methods
We compared the effectiveness of inhaled tiotropium bromide for 2 months between pre- and post-treatment pulmonary function tests performed on 29 patients with destroyed lung due to TB.
Results
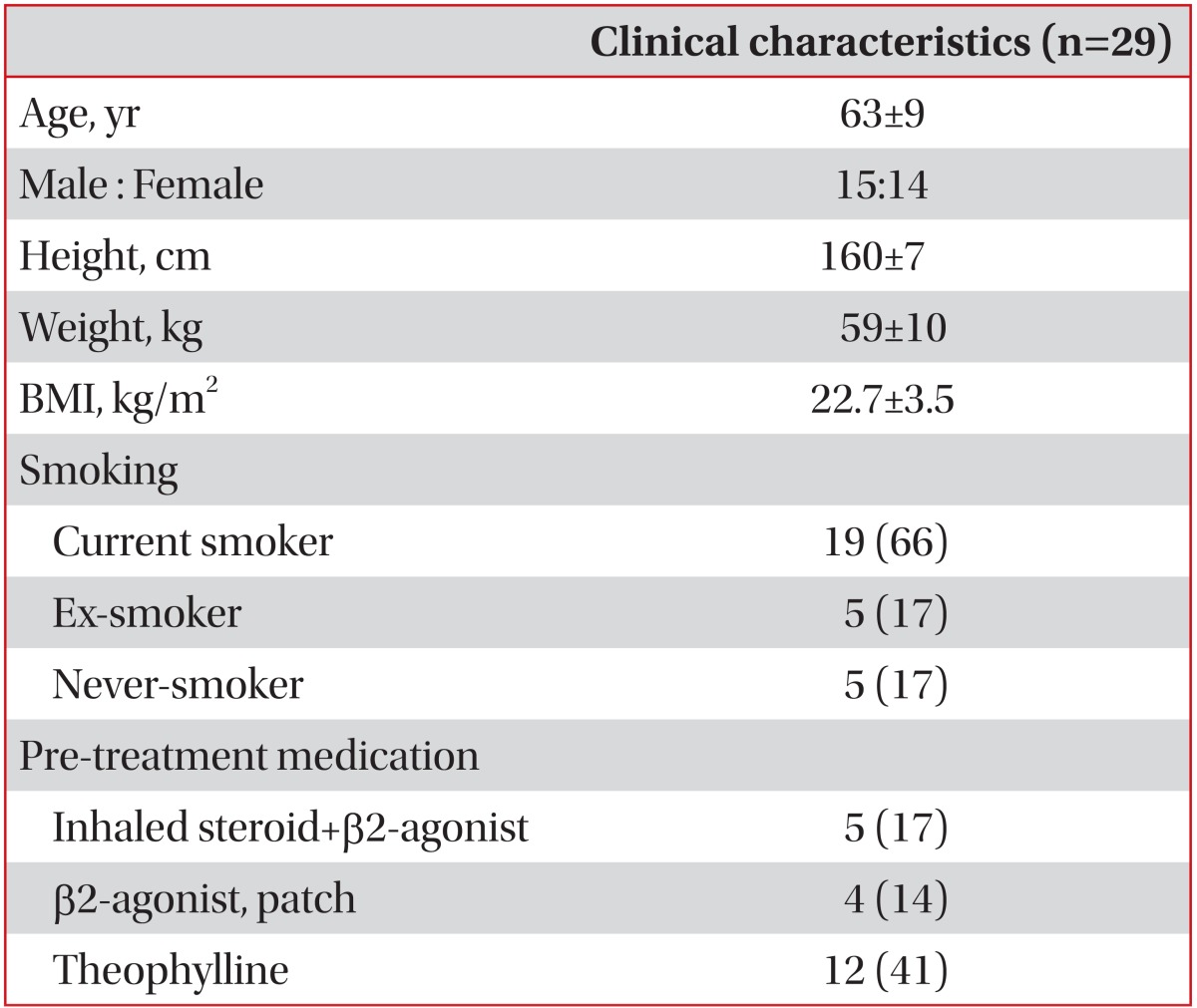
The mean age of the total number of patients was 63±9 years, where 15 patients were male. The pre-treatment mean forced expiratory volume in 1 second (FEV1) was 1.02±0.31 L (44.1±16.0% predicted). The pre-treatment mean forced vital capacity (FVC) was 1.70±0.54 L (52.2±15.8% predicted). Overall, the change in FEV1% predicted over baseline with tiotropium was 19.5±19.1% (p<0.001). Twenty patients (72%) got better than a 10% increase in FEV1 over baseline with tiotropium, but one patient showed more than a 10% decrease in FEV1. Overall, the change in FVC% predicted over baseline with tiotropium was 18.5±19.9% (p<0.001). Seventeen patients (59%) experienced greater than a 10% increase in FVC over baseline with tiotropium; 12 (41%) patients had stable lung function.
Pulmonary tuberculosis (TB) is a common disease that can result in residual anatomic and functional changes in the lung despite microbiological cure. Bronchial and parenchymal structural changes result in sequelae, including bronchovascular distortion, fibrotic bands, emphysematous changes, and bronchiectasis1. These sequelae are associated with pulmonary impairment after TB that occurs frequently and varies from mild to severe. In particular, damage to bronchi results from extensive fibrosis or endobronchial stricture, as tuberculous sequelae cause airflow obstruction2,3,4,5,6,7,8,9.
Studies regarding pulmonary function in individuals with pulmonary TB demonstrated restrictive, obstructive, or mixed patterns and range from normal to severe impairment8,10,11. Although accurate estimates of the frequency and extent of pulmonary impairment from TB are unknown, in a recent study, over half of all treated pulmonary TB patients in Tarrant Country had significantly impaired pulmonary functions7. However, there is currently no effective treatment, which is urgently required in patients with secondary airflow obstruction.
Tiotropium is an inhaled anti-cholinergic agent that has been used as a bronchodilator in patients with chronic obstructive pulmonary disease (COPD). The parasympathetic activity in the airway induces bronchial smooth muscle contraction and mucus production via the muscarinic receptors located on smooth muscle cells and within the submucosal glands. Tiotropium acts as a muscarinic receptor antagonist that is able to improve airway limitations while also suppressing airway secretion12,13,14.
In Korea, the incidence of TB is within the intermediate range15, where patients with destroyed lung due to TB accounts for a significant portion of those patients with chronic airflow obstruction, treatment guidelines for those with secondary airflow obstruction may be confused with those of COPD. Occasionally, tiotropium was administered to patients with destroyed lung due to TB. The aim of this study was to evaluate the efficacy of inhaled tiotropium bromide in tuberculous destroyed lung.
Pulmonary function tests can objectively quantify lung function and have been used as the standard evaluation of impairment from chronic lung disease. To evaluate the efficacy of inhaled tiotropium bromide in tuberculous destroyed lung, we compared pre-treatment and post-treatment pulmonary function tests of patients with destroyed lung due to TB.
Initial and serial pulmonary function tests of patients with tuberculous destroyed lung who inhaled tiotropium bromide as a treatment were retrospectively analyzed from 2007 through 2009. A total of 29 patients were enrolled. The study subjects were patients who visited Seoul Paik Hospital, Inje University, and presented with dyspnea and/or cough and sputum. Subjects had a forced expiratory volume in 1 second (FEV1)<80% of the predicted value at pre-treatment pulmonary function test. Inhaled tiotropium bromide was administered 18 µg once daily for 2 months. We defined TB destroyed lung patients as presenting with lung function insufficiency due to parenchymal damage to more than 1/2 of one lung with a history of TB and no current evidence of active TB. Based on the smoking histories, "never-smokers" were defined as those who had smoked on average<1 cigarette per day for <6 months or had never smoked.
Spirometry was measured by using the Vmax22 (Sensor-Medics Co., Yorva Linda, CA, USA). In order to evaluate the bronchodilator response, we used a beta-2 agonist (salbutamol, 100 µg). Positive bronchodilator response was defined using the criteria after bronchodilator inhalation, when absolute change of FEV1 was more than 0.2 L and a percentage of initial FEV1 was more than 12%.
Changes in pulmonary function tests were presented as the percentage change of initial value. Considering restrictive, obstructive, or mixed lung function patterns in patients with TB destroyed lung, improvements and deteriorations were defined as >10% changes in pulmonary function tests16. Patients who did not demonstrate improvement or deterioration were considered stable. Also changes in FEV1, forced vital capacity (FVC) over time and correlation with initial FEV1 were analyzed.
All data were expressed as means and standard deviations or frequencies. Statistical analysis was performed using SPSS-PC non-parametrically. The Wilcoxon signed rank test was used to compare data in paired samples, and the McNemar test to analyze categorical variables in paired samples. Statistical significance was accepted for p-values less than 0.05.
The baseline clinical characteristics of study patients are given in Table 1. Of the 29 patients, 20 (69%) had FEV1/FVC ratio of <0.7. The pre-treatment mean FEV1 was 1.02±0.31 L (44.1±16.0% predicted). The pre-treatment mean FVC was 1.70±0.54 L (52.2±15.8% predicted). At baseline, 4 patients (14%) showed more than a 12% increase in FEV1 with salbutamol but none of them showed more than a 200 mL increase. Prior all medications including bronchodilators were not changed. None of the participating subjects developed an acute exacerbation of respiratory symptoms or serious adverse events during the study period.
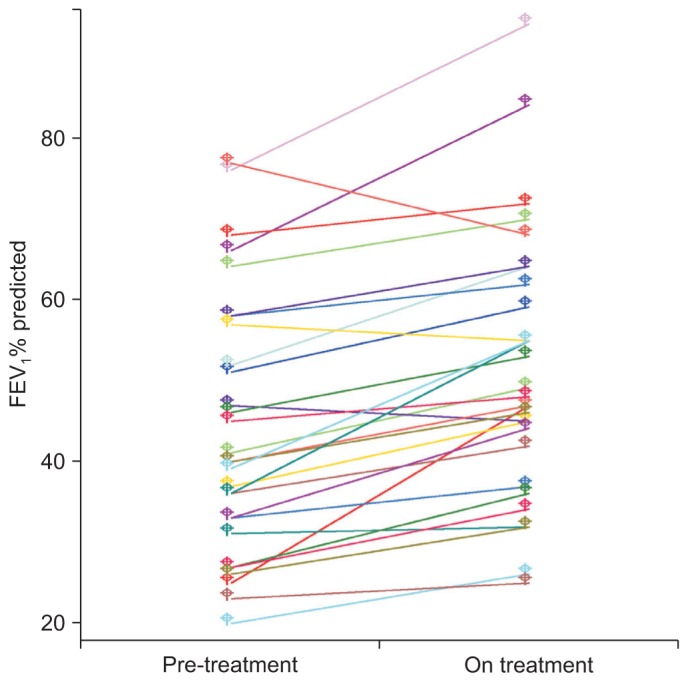
Treatment with tiotropium resulted in comparable bronchodilation compared with baseline, as measured by all the spirometric parameters. Paired quantitative FEV1% predicted pre-treatment and on treatment was shown in Figure 1. Overall change in FEV1 response with tiotropium was 0.16±0.15 L (7.3±6.7%) (p<0.001), while the change in FEV1% predicted over baseline was 19.5±19.1%. Twenty patients (72%) got better than a 10% increase in FEV1 over baseline with tiotropium, but one patient showed more than a 10% decrease in FEV1. Overall change in FVC response with tiotropium was 0.27±0.31 L (8.2±8.8%) (p<0.001), while the change in FVC% predicted over baseline was 18.5±19.9%. Seventeen patients (59%) experienced greater than a 10% increase in FVC over baseline with tiotropium; 12(41%) patients had stable lung function. In addition, irrespective of FEV1/FVC ratio (obstructive or nonobstructive patterns), FEV1 and FVC improved significantly (p<0.05). Also FEV1 and FVC improved significantly (p<0.05) in smoker and never-smokers, although there were small numbers of never-smokers.
Figure 2 reflected means (±SE) of FEV1 and FVC% predicted changes from baseline according to the initial FEV1 level. Changes in FEV1 and FVC% predicted over baseline were negatively correlated with initial FEV1 level (γ=-0.472, p=0.010 and γ=-0.483, p=0.008, respectively).
In this study, of the 29 patients, 20 had FEV1/FVC ratio of <0.7. Irrespective of FEV1/FVC ratio, FEV1 and FVC improved significantly with inhaled tiotropium in patients with TB destroyed lung. These data suggest that inhaled tiotropium bromide therapy may lead to improved lung functions in patients with TB destroyed lung.
TB and COPD carry a significant burden in terms of morbidity and mortality worldwide. The development and subsequent disease progression seen both in TB and COPD result in characteristic destructive parenchymal lung changes. A common link to the pathogenesis of both conditions may lie in the destruction of the pulmonary extra-cellular matrix comprised of collagen and elastin which is key to the structural integrity of the lung5,17. In particular, extensive parenchymal lung destruction through the dysregulation of matrix metalloproteinases by TB has been demonstrated18.
The development of chronic airflow obstruction and respiratory symptoms may be preceded by one or several episodes of active TB. In a recent study performed in China, prior pulmonary TB had been demonstrated to be associated with a higher risk of airflow obstruction (odds ratio, 1.37; 95% confidence interval, 1.13-1.67), irrespective of smoking status5. In one of the case-control studies, individuals who had been treated for TB had significantly lower FEV1 levels than the matched healthy controls10. In another study, the percentage of subjects with chronic airflow impairment (FEV1 80% predicted) was 18.4% in those with one episode, 27.1% in those with two, and 35.2% in those with three or more episodes of TB19. In patients with TB destroyed lung, the degree of impairment was variable, ranging from mild to severe. Due to the presence of extensive lesions, pulmonary restriction and obstruction with low vital capacity were the predominant patterns observed7.
There is currently no standard treatment or study for patients with secondary airflow obstruction. In chronic bronchitis, anti-cholinergic drugs are as effective bronchodilators as are sympathomimetics, suggesting a mechanism of vagally-mediated reflex bronchoconstriction. In 1979, a single-blind, cross-over comparison of standard doses of ipratropium bromide and fenoterol in 36 patients of experiments in 6 patients with partially reversible airway obstruction, secondary to chronic pulmonary TB, revealed no difference between the effect of bronchodilating drugs, evaluated by spirometry. Authors proposed that a vagal reflex mechanism plays a major role in bronchoconstriction connected with severe chronic pulmonary TB20. In a more recent study, tiotropium improved the symptoms of cough, sputum and breathlessness in the macrolide-resistant cases of diffuse panbronchiolitis, bronchiectasis and sinobronchial syndrome. Also FEV1 value was significantly improved after 3 months of treatment with tiotropium (mean improvement in FEV1 0.11 L, p=0.016). The authors insisted that these beneficial effects may have been due to the suppression of air way secretion through the anti-cholinergic effect of tiotropium on the submucosal gland12. Their pulmonary functions test showed a mild but significant improvement in the FEV1 and FVC after treatment with tiotropium. It is probable that relaxation of bronchial smooth muscle and/or reduction of airway secretion by tiotropium might improve pulmonary functions in patients with TB destroyed lung.
This study has several limitations. First, the number of cases involved was small. Especially, due to small number of never-smokers, when the patients were divided into two groups by smoking status, there was no significant difference of effect of inhaled tiotropium on spirometric parameters in patients with tuberculous destroyed lung. Also among smokers, we could not find evidence of a dose-response relationship between increasing pack-years of exposure and pulmonary impairment. However, our founding is in accordance with previous cross-sectional study5 conducted in TB patients. Lam et al.5 found that prior TB is an independent risk factor for airflow obstruction irrespective of smoking status. Second, the improvement in the pulmonary function test was only with regards to the short-term observations of this study. Therefore, the long-term effectiveness of this treatment needs to be further assessed. Third, although tiotropium improved the subjective symptoms of dyspnea, cough and sputum, in most of patients with TB destroyed lung, symptoms were not evaluated by instrument or scale. Last, this study is not a prospective, randomized study. However, there is no study that outlined treatment guidelines for patients with destroyed lung due to TB, which accounts for a significant portion of those with chronic airflow obstruction. To our knowledge, this is first study for treating patients with TB destroyed lung in spite of these limitations.
In conclusion, we were able to demonstrate that the inhalation of tiotropium has a significant effect on spirometric parameters in patients with TB destroyed lung. Therefore, large scale prospective and controlled studies should be performed to establish the efficacy of tiotropium on the long-term prognosis in patients with TB destroyed lung.
References
1. Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH. Thoracic sequelae and complications of tuberculosis. Radiographics 2001;21:839-858. PMID: 11452057.


2. Ramos LM, Sulmonett N, Ferreira CS, Henriques JF, de Miranda SS. Functional profile of patients with tuberculosis sequelae in a university hospital. J Bras Pneumol 2006;32:43-47. PMID: 17273568.



3. Plit ML, Anderson R, Van Rensburg CE, Page-Shipp L, Blott JA, Fresen JL, et al. Influence of antimicrobial chemotherapy on spirometric parameters and pro-inflammatory indices in severe pulmonary tuberculosis. Eur Respir J 1998;12:351-356. PMID: 9727784.


4. Lee JH, Chang JH. Lung function in patients with chronic airflow obstruction due to tuberculous destroyed lung. Respir Med 2003;97:1237-1242. PMID: 14635980.


5. Lam KB, Jiang CQ, Jordan RE, Miller MR, Zhang WS, Cheng KK, et al. Prior TB, smoking, and airflow obstruction: a cross-sectional analysis of the Guangzhou Biobank Cohort Study. Chest 2010;137:593-600. PMID: 19820078.


6. Pasipanodya JG, Miller TL, Vecino M, Munguia G, Bae S, Drewyer G, et al. Using the St. George respiratory questionnaire to ascertain health quality in persons with treated pulmonary tuberculosis. Chest 2007;132:1591-1598. PMID: 17890471.


7. Pasipanodya JG, Miller TL, Vecino M, Munguia G, Garmon R, Bae S, et al. Pulmonary impairment after tuberculosis. Chest 2007;131:1817-1824. PMID: 17400690.


8. Long R, Maycher B, Dhar A, Manfreda J, Hershfield E, Anthonisen N. Pulmonary tuberculosis treated with directly observed therapy: serial changes in lung structure and function. Chest 1998;113:933-943. PMID: 9554628.


9. Menezes AM, Hallal PC, Perez-Padilla R, Jardim JR, Muino A, Lopez MV, et al. Tuberculosis and airflow obstruction: evidence from the PLATINO study in Latin America. Eur Respir J 2007;30:1180-1185. PMID: 17804445.


10. Willcox PA, Ferguson AD. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir Med 1989;83:195-198. PMID: 2595036.


11. Snider GL, Doctor L, Demas TA, Shaw AR. Obstructive airway disease in patients with treated pulmonary tuberculosis. Am Rev Respir Dis 1971;103:625-640. PMID: 5579906.

12. Saito Y, Azuma A, Morimoto T, Fujita K, Abe S, Motegi T, et al. Tiotropium ameliorates symptoms in patients with chronic airway mucus hypersecretion which is resistant to macrolide therapy. Intern Med 2008;47:585-591. PMID: 18379141.


13. Maesen FP, Smeets JJ, Sledsens TJ, Wald FD, Cornelissen PJ. Dutch Study Group. Tiotropium bromide, a new long-acting antimuscarinic bronchodilator: a pharmacodynamic study in patients with chronic obstructive pulmonary disease (COPD). Eur Respir J 1995;8:1506-1513. PMID: 8575576.


14. Celli BR, MacNee W. ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004;23:932-946. PMID: 15219010.


15. World Health Organization. Global tuberculosis control: surveillance, planning, financing: WHO report 2006. Geneva: World Health Organization; 2008.
16. American Thoracic Society. American Thoracic Society (ATS). the European Respiratory Society (ERS). Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. Am J Respir Crit Care Med 2000;161(2 Pt 1):646-664. PMID: 10673212.


17. Chakrabarti B, Calverley PM, Davies PD. Tuberculosis and its incidence, special nature, and relationship with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2007;2:263-272. PMID: 18229564.


18. Elkington PT, Friedland JS. Matrix metalloproteinases in destructive pulmonary pathology. Thorax 2006;61:259-266. PMID: 16227332.



19. Hnizdo E, Singh T, Churchyard G. Chronic pulmonary function impairment caused by initial and recurrent pulmonary tuberculosis following treatment. Thorax 2000;55:32-38. PMID: 10607799.



20. Salorinne Y, Stenius-Aarniala B, Poppius H. Effect of ipratropium bromide and fenoterol on airway obstruction in chronic pulmonary tuberculosis. Respiration 1979;38:151-154. PMID: 160068.


Figure 1
Paired quantitative forced expiratory volume in 1 second (FEV1) % predicted pre-treatment and on treatment. Overall, the change in FEV1% predicted with tiotropium over baseline was 19.5±19.1% (p<0.001).
- TOOLS
-
METRICS

- Related articles
-
Superoxide Generation by Bronchoalveolar Lavage Cells in Patients with Tuberculosis1990 March;37(1)



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



