 |
 |
| Tuberc Respir Dis > Volume 80(1); 2017 > Article |
|
Tuberculous pleurisy is the most common form of extrapulmonary tuberculosis (TB) and is the main cause of pleural effusion in Korea1,2. In Korea, 3,089 new tuberculous pleurisy cases were reported in 2015, which accounted for 9.6% of the 32,181 new TB cases and 46.6% of the 6,631 extrapulmonary TB cases (Table 1)3.
Traditionally, tuberculous pleurisy is indicated by predominant lymphocytosis in the pleural fluid and a low yield of effusion culture due to the paucibacillary nature of TB4. However, several recent studies have reported that the lymphocyte counts in pleural fluid were decreased in patients who were diagnosed with tuberculous pleurisy, and 10%-17% of the patients with tuberculous pleurisy had neutrophil-predominant pleural fluid5,6,7,8. In addition, the yield of effusion culture is reported to be higher (15%-63%) than previously thought, with the introduction of a liquid culture method, and the lymphocyte percentage in pleural fluid was negatively associated with the probability of a positive effusion culture6,7,8,9.
The radiographic appearances of tuberculous pleurisy can be subdivided into two types, based on the chest X-ray, chest computed tomography, or chest ultrasonography findings: free-flowing and loculated effusions10,11. Residual pleural thickening is a common complication of tuberculous pleurisy, and a loculated effusion at the initial presentation was associated with significant residual pleural thickening12,13. Intrapleural fibrinolytic therapy can reduce this residual pleural thickening in patients with loculated tuberculous pleurisy10,14. In comparison, the characteristics of the effusion in loculated tuberculous pleurisy have not been well studied.
In this issue of Tuberculosis and Respiratory Diseases, Ko et al.15 described the pleural fluid characteristics in patients with tuberculous pleurisy to examine the association between loculation and positive mycobacterial cultures of pleural fluid. Among 219 patients with tuberculous pleurisy, loculation was identified in 86 patients (39%), and 69 patients (32%) had effusion cultures positive for Mycobacterium tuberculosis. The proportion of loculation was much higher in the patients with positive effusion cultures (86%, 59/69) than in the patients with negative effusion cultures (18%, 27/150). In other words, the majority of patients (69%, 59/86) with loculated tuberculous pleurisy had positive effusion cultures, whereas positive effusion cultures were found only in 7.5% of the patients (10/133) without loculation. In their study, nine patients had neutrophil-predominant pleural effusions. All of them were culture positive for M. tuberculosis in pleural fluid, and six of them had loculated tuberculous pleurisy. Compared to the patients with negative effusion cultures, those with positive effusion cultures had a lower lymphocyte percentage, pH, and glucose level and a higher neutrophil percentage and higher protein and lactate dehydrogenase (LDH) levels in the pleural effusion, and higher serum C-reactive protein levels. Multiple logistic regression analysis found that loculation of the pleural fluid (adjusted odds ratio [OR], 40.06; 95% confidence interval [CI], 9.36-171.56; p<0.001) was associated, and lymphocyte percentage was inversely associated (adjusted OR, 0.93; 95% CI, 0.90-0.97; p=0.001) with a positive effusion culture.
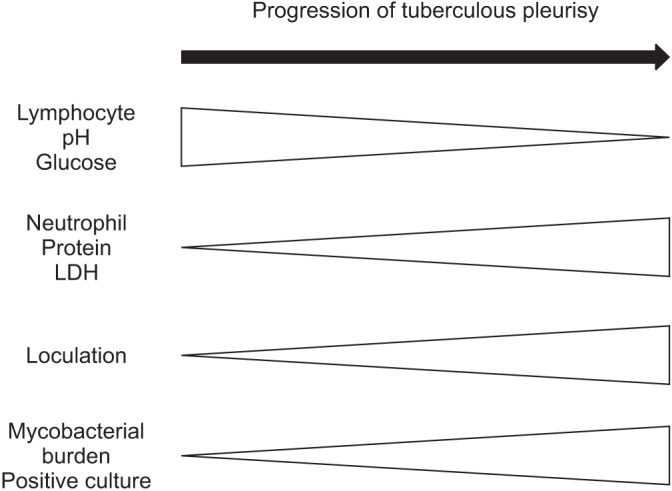
The traditional concept of the pathogenesis of tuberculous pleurisy is rupture of a subpleural caseous focus followed by a delayed hypersensitivity reaction to M. tuberculosis antigens1. These occurrences result in lymphocyte-predominance and a low yield of effusion culture in tuberculous pleurisy6. However, tuberculous pleurisy may involve a continuous spectrum of disease processes (Figure 1). In the early phase of tuberculous pleurisy, the pleural effusion could have lymphocyte-predominance, a high pH, and high glucose levels. As the tuberculous pleurisy progresses, the pleural effusion could develop neutrophil-predominance, and high protein and LDH levels, as well as loculation and positive effusion cultures, as found in Ko et al.15.
From a clinical perspective, Ko et al.15 indicated that suspicion and the differentiation of tuberculous pleurisy from a parapneumonic effusion are very important in patients with loculated pleural effusions. Loculated pleural effusions, especially neutrophil-predominant effusions, are typically considered to be parapneumonic effusions in clinical practice. The inclusion of tuberculous pleurisy in the differential diagnosis and prompt sputum and pleural fluid examination for possible tuberculous pleurisy are needed, especially in TB-endemic areas.
References
3. Korean Centers for Disease Control and Prevention. Notified tuberculosis status in Korea [Internet]. Cheongju: Centers for Disease Control and Prevention; 2015. cited 2016 Dec 10. Available from: http://cdc.go.kr/CDC/cms/content/mobile/45/67545_view.html.
5. Lin MT, Wang JY, Yu CJ, Lee LN, Yang PC. TAMI Group. Mycobacterium tuberculosis and polymorphonuclear pleural effusion: incidence and clinical pointers. Respir Med 2009;103:820-826. PMID: 19217271.


6. Ruan SY, Chuang YC, Wang JY, Lin JW, Chien JY, Huang CT, et al. Revisiting tuberculous pleurisy: pleural fluid characteristics and diagnostic yield of mycobacterial culture in an endemic area. Thorax 2012;67:822-827. PMID: 22436167.



7. Bielsa S, Palma R, Pardina M, Esquerda A, Light RW, Porcel JM. Comparison of polymorphonuclear- and lymphocyterich tuberculous pleural effusions. Int J Tuberc Lung Dis 2013;17:85-89. PMID: 23164256.


8. Choi H, Chon HR, Kim K, Kim S, Oh KJ, Jeong SH, et al. Clinical and laboratory differences between lymphocyte- and neutrophil-predominant pleural tuberculosis. PLoS One 2016;11:e0165428PMID: 27788218.



9. Liu SF, Liu JW, Lin MC. Characteristics of patients suffering from tuberculous pleuritis with pleural effusion culture positive and negative for Mycobacterium tuberculosis, and risk factors for fatality. Int J Tuberc Lung Dis 2005;9:111-115. PMID: 15675559.

10. Chung CL, Chen CH, Yeh CY, Sheu JR, Chang SC. Early effective drainage in the treatment of loculated tuberculous pleurisy. Eur Respir J 2008;31:1261-1267. PMID: 18216051.


11. Cao GQ, Li L, Wang YB, Shi ZZ, Fan DY, Chen HY. Treatment of free-flowing tuberculous pleurisy with intrapleural urokinase. Int J Tuberc Lung Dis 2015;19:1395-1400. PMID: 26467594.


12. Barbas CS, Cukier A, de Varvalho CR, Barbas Filho JV, Light RW. The relationship between pleural fluid findings and the development of pleural thickening in patients with pleural tuberculosis. Chest 1991;100:1264-1267. PMID: 1935279.


13. Han DH, Song JW, Chung HS, Lee JH. Resolution of residual pleural disease according to time course in tuberculous pleurisy during and after the termination of antituberculosis medication. Chest 2005;128:3240-3245. PMID: 16304268.


14. Kwak SM, Park CS, Cho JH, Ryu JS, Kim SK, Chang J, et al. The effects of urokinase instillation therapy via percutaneous transthoracic catheter in loculated tuberculous pleural effusion: a randomized prospective study. Yonsei Med J 2004;45:822-828. PMID: 15515192.


Table 1
Tuberculous pleurisy in Korea (2005-2015)
- TOOLS


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation




