1. Velayati AA, Farnia P, Masjedi MR. Latent tuberculosis (TB) bacilli: yes or no to preventive chemotherapy. Int J Mycobacteriol 2012;1:1-2.


2. Hibah NA, Hasan HE. Prevalence of latent tuberculosis infection among multinational healthcare workers in Muhayil Saudi Arabia. Egypt J Bronchol 2015;9:183-7.

4. World Health Organization. Latent TB infection: updated and consolidated guidelines for programmatic management. Geneva: World Health Organization; 2018.
6. Daniel TM. The history of tuberculosis. Respir Med 2006;100:1862-70.


7. Grosset J. The sterilizing value of rifampicin and pyrazinamide in experimental short-course chemotherapy. Bull Int Union Tuberc 1978;53:5-12.


8. Wayne LG. Dormancy of
Mycobacterium tuberculosis and latency of disease. Eur J Clin Microbiol Infect Dis 1994;13:908-14.



9. Agarwal R. Treatment of latent tuberculous infection in India: is it worth the salt? Lung India 2005;22:105-6.
10. Huaman MA, Ticona E, Miranda G, Kryscio RJ, Mugruza R, Aranda E, et al. The relationship between latent tuberculosis infection and acute myocardial infarction. Clin Infect Dis 2018;66:886-92.


11. Velayati AA, Abeel T, Shea T, Konstantinovich Zhavnerko G, Birren B, Cassell GH, et al. Populations of latent
Mycobacterium tuberculosis lack a cell wall: Isolation, visualization, and whole-genome characterization. Int J Mycobacteriol 2016;5:66-73.


13. Adeiza MA. Diagnosis of latent tuberculosis infection: the tuberculin skin test and interferon gamma release assays. Ann Niger Med 2011;5:35-7.

14. Zondervan NA, van Dam JC, Schaap PJ, Martins Dos Santos VA, Suarez-Diez M. Regulation of three virulence strategies of
Mycobacterium tuberculosis: a success story. Int J Mol Sci 2018;19:347.



15. Welin A. Survival strategies of Mycobacterium tuberculosis inside the human macrophage. Linköping: Linköping University; 2011.
16. Curcic R, Dhandayuthapani S, Deretic V. Gene expression in mycobacteria: transcriptional fusions based on xylE and analysis of the promoter region of the response regulator mtrA from
Mycobacterium tuberculosis. Mol Microbiol 1994;13:1057-64.


17. O’Neill MB, Mortimer TD, Pepperell CS. Diversity of
Mycobacterium tuberculosis across Evolutionary Scales. PLoS Pathog 2015;11:e1005257.



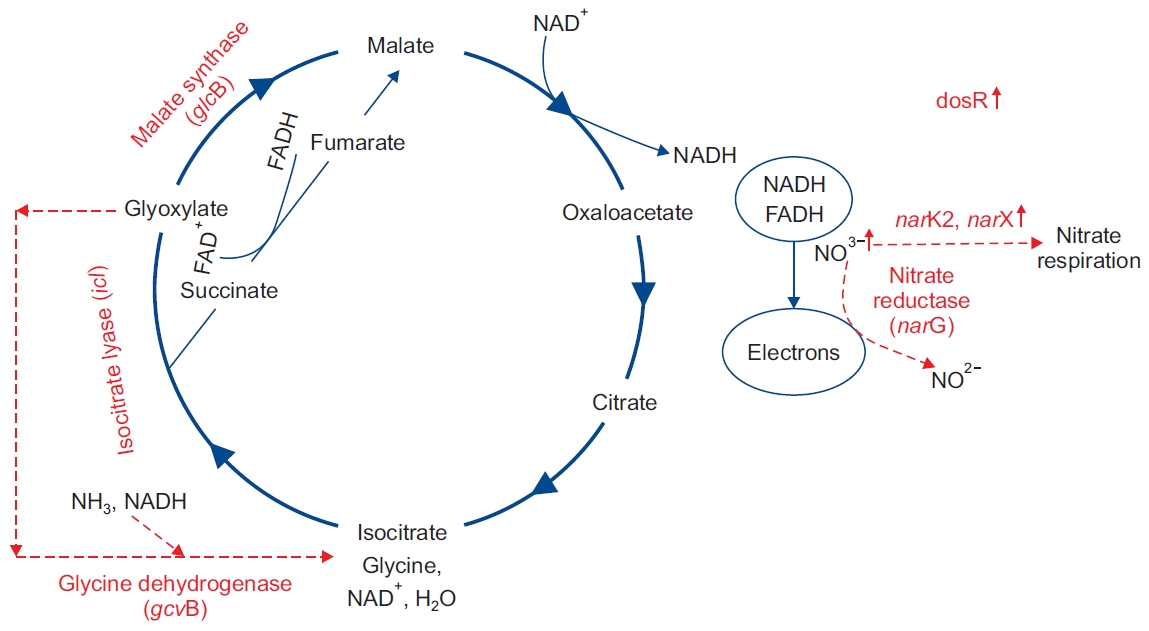
19. Voskuil MI, Visconti KC, Schoolnik GK.
Mycobacterium tuberculosis gene expression during adaptation to stationary phase and low-oxygen dormancy. Tuberculosis (Edinb) 2004;84:218-27.


20. Lancaster CR, Kroger A. Succinate: quinone oxidoreductases: new insights from X-ray crystal structures. Biochim Biophys Acta 2000;1459:422-31.


21. Kana BD, Weinstein EA, Avarbock D, Dawes SS, Rubin H, Mizrahi V. Characterization of the cydAB-encoded cytochrome bd oxidase from
Mycobacterium smegmatis. J Bacteriol 2001;183:7076-86.



22. Cole ST, Brosch R, Parkhill J, Garnier T, Churcher C, Harris D, et al. Deciphering the biology of
Mycobacterium tuberculosis from the complete genome sequence. Nature 1998;393:537-44.


23. Pham TV, Murkin AS, Moynihan MM, Harris L, Tyler PC, Shetty N, et al. Mechanism-based inactivator of isocitrate lyases 1 and 2 from
Mycobacterium tuberculosis. Proc Natl Acad Sci U S A 2017;114:7617-22.



24. Neidhardt FC, Curtiss R. Escherichia coli and Salmonella: cellular and molecular biology. Washington, DC: ASM Press; 1996. p. 1227-3122.
25. Kumar R, Bhakuni V.
Mycobacterium tuberculosis isocitrate lyase (MtbIcl): role of divalent cations in modulation of functional and structural properties. Proteins 2008;72:892-900.


26. Smith CV, Huang CC, Miczak A, Russell DG, Sacchettini JC, Honer zu Bentrup K. Biochemical and structural studies of malate synthase from
Mycobacterium tuberculosis. J Biol Chem 2003;278:1735-43.


27. Gengenbacher M, Kaufmann SH.
Mycobacterium tuberculosis : success through dormancy. FEMS Microbiol Rev 2012;36:514-32.



28. Ellenbarger JF, Krieger IV, Huang HL, Gomez-Coca S, Ioerger TR, Sacchettini JC, et al. Anion-pi interactions in computer-aided drug design: modeling the inhibition of malate synthase by phenyl-diketo acids. J Chem Inf Model 2018;58:2085-91.


29. Wayne LG, Sohaskey CD. Nonreplicating persistence of mycobacterium tuberculosis. Annu Rev Microbiol 2001;55:139-63.


30. Huang HL, Krieger IV, Parai MK, Gawandi VB, Sacchettini JC.
Mycobacterium tuberculosis malate synthase structures with fragments reveal a portal for substrate/product exchange. J Biol Chem 2016;291:27421-32.



31. Kelkar DS, Kumar D, Kumar P, Balakrishnan L, Muthusamy B, Yadav AK, et al. Proteogenomic analysis of
Mycobacterium tuberculosis by high resolution mass spectrometry. Mol Cell Proteomics 2011;10:M111.011627.



33. Parrish NM, Dick JD, Bishai WR. Mechanisms of latency in
Mycobacterium tuberculosis. Trends Microbiol 1998;6:107-12.


34. Wayne LG, Hayes LG. Nitrate reduction as a marker for hypoxic shiftdown of
Mycobacterium tuberculosis. Tuber Lung Dis 1998;79:127-32.


35. Sohaskey CD, Wayne LG. Role of narK2X and narGHJI in hypoxic upregulation of nitrate reduction by
Mycobacterium tuberculosis. J Bacteriol 2003;185:7247-56.



36. Sohaskey CD. Nitrate enhances the survival of
Mycobacterium tuberculosis during inhibition of respiration. J Bacteriol 2008;190:2981-6.



37. Sohaskey CD. Regulation of nitrate reductase activity in
Mycobacterium tuberculosis by oxygen and nitric oxide. Microbiology (Reading) 2005;151:3803-10.


38. Black GF, Thiel BA, Ota MO, Parida SK, Adegbola R, Boom WH, et al. Immunogenicity of novel DosR regulon-encoded candidate antigens of
Mycobacterium tuberculosis in three high-burden populations in Africa. Clin Vaccine Immunol 2009;16:1203-12.



39. Hutter B, Dick T. Analysis of the dormancy-inducible narK2 promoter in
Mycobacterium bovis BCG. FEMS Microbiol Lett 2000;188:141-6.


40. Sohaskey CD, Modesti L. Differences in nitrate reduction between
Mycobacterium tuberculosis and
Mycobacterium bovis are due to differential expression of both narGHJI and narK2. FEMS Microbiol Lett 2009;290:129-34.


41. Honaker RW, Stewart A, Schittone S, Izzo A, Klein MR, Voskuil MI.
Mycobacterium bovis BCG vaccine strains lack narK2 and narX induction and exhibit altered phenotypes during dormancy. Infect Immun 2008;76:2587-93.



42. Giffin MM, Raab RW, Morganstern M, Sohaskey CD. Mutational analysis of the respiratory nitrate transporter NarK2 of
Mycobacterium tuberculosis. PLoS One 2012;7:e45459.



43. Kendall SL, Movahedzadeh F, Rison SC, Wernisch L, Parish T, Duncan K, et al. The
Mycobacterium tuberculosis dosRS two-component system is induced by multiple stresses. Tuberculosis (Edinb) 2004;84:247-55.


44. Hutter B, Dick T. Up-regulation of narX, encoding a putative ‘fused nitrate reductase’ in anaerobic dormant
Mycobacterium bovis BCG. FEMS Microbiol Lett 1999;178:63-9.


45. Fenhalls G, Stevens L, Moses L, Bezuidenhout J, Betts JC, van Helden P, et al. In situ detection of
Mycobacterium tuberculosis transcripts in human lung granulomas reveals differential gene expression in necrotic lesions. Infect Immun 2002;70:6330-8.



46. Queiroz A, Riley LW. Bacterial immunostat:
Mycobacterium tuberculosis lipids and their role in the host immune response. Rev Soc Bras Med Trop 2017;50:9-18.


50. Huang CC, Smith CV, Glickman MS, Jacobs WR Jr, Sacchettini JC. Crystal structures of mycolic acid cyclopropane synthases from
Mycobacterium tuberculosis. J Biol Chem 2002;277:11559-69.


51. PupMed. pcaA: cyclopropane mycolic acid synthase (Mycobacterium tuberculosis H37Rv). Bethesda: National Library of Medicine; 2018.
52. Corrales RM, Molle V, Leiba J, Mourey L, de Chastellier C, Kremer L. Phosphorylation of mycobacterial PcaA inhibits mycolic acid cyclopropanation: consequences for intracellular survival and for phagosome maturation block. J Biol Chem 2012;287:26187-99.


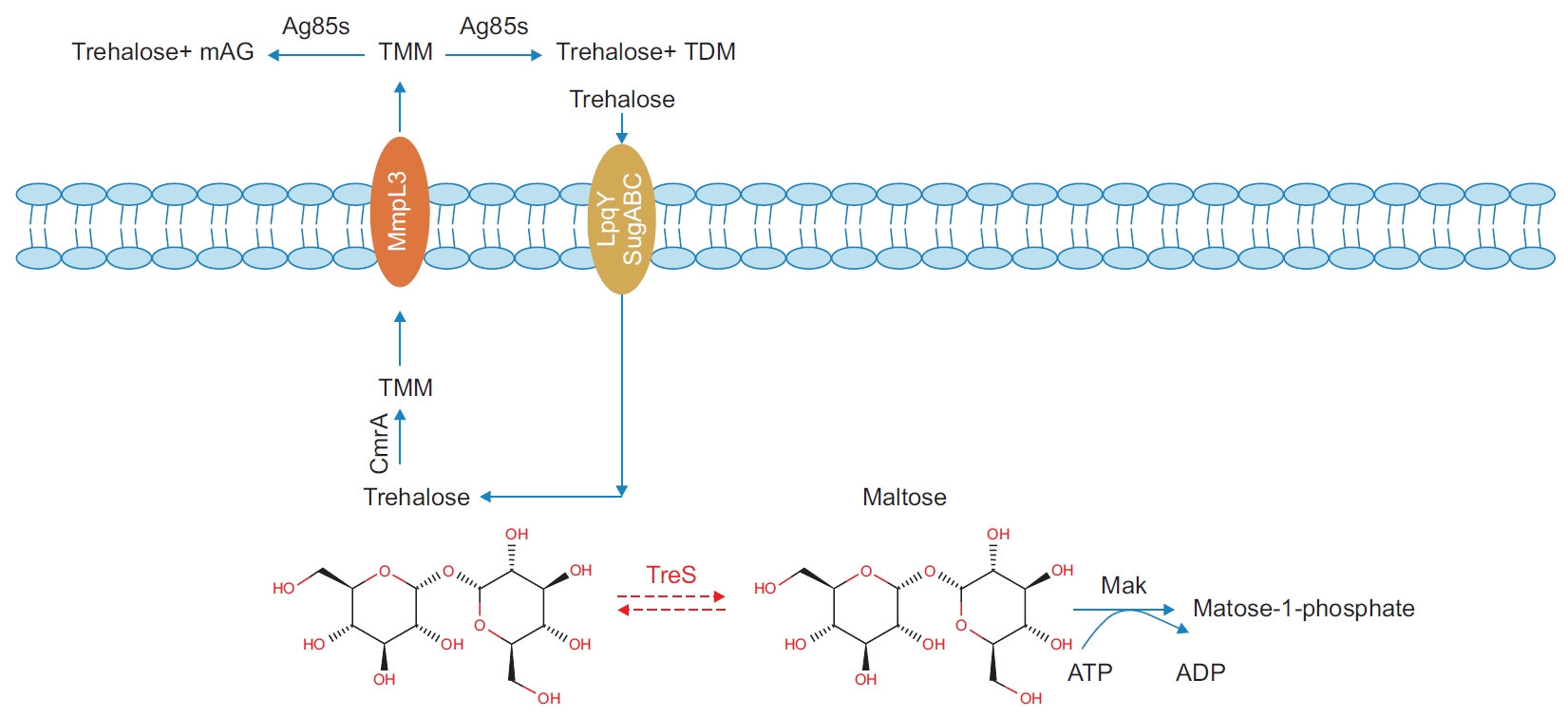
53. Nishimoto T, Nakano M, Nakada T, Chaen H, Fukuda S, Sugimoto T, et al. Purification and properties of a novel enzyme, trehalose synthase, from Pimelobacter sp. R48. Biosci Biotechnol Biochem 1996;60:640-4.


54. Caner S, Nguyen N, Aguda A, Zhang R, Pan YT, Withers SG, et al. The structure of the
Mycobacterium smegmatis trehalose synthase reveals an unusual active site configuration and acarbose-binding mode. Glycobiology 2013;23:1075-83.



55. Umesiri FE, Sanki AK, Boucau J, Ronning DR, Sucheck SJ. Recent advances toward the inhibition of mAG and LAM synthesis in
Mycobacterium tuberculosis. Med Res Rev 2010;30:290-326.


56. Thanna S, Sucheck SJ. Targeting the trehalose utilization pathways of
Mycobacterium tuberculosis. Medchemcomm 2016;7:69-85.


57. Zahrt TC, Deretic V.
Mycobacterium tuberculosis signal transduction system required for persistent infections. Proc Natl Acad Sci U S A 2001;98:12706-11.



58. Marszalek M, Planas A, Pellicer T. Two-component systems of Mycobacterium tuberculosis as potential targets for drug development. Afinidad 2014;71:172-8.
60. Jordan S, Hutchings MI, Mascher T. Cell envelope stress response in Gram-positive bacteria. FEMS Microbiol Rev 2008;32:107-46.


61. Zhou P, Long Q, Zhou Y, Wang H, Xie J.
Mycobacterium tuberculosis two-component systems and implications in novel vaccines and drugs. Crit Rev Eukaryot Gene Expr 2012;22:37-52.


62. Tyagi JS, Sharma D. Signal transduction systems of mycobacteria with special reference to M. tuberculosis. Curr Sci 2004;86:93-102.
63. Wisedchaisri G, Wu M, Sherman DR, Hol WG. Crystal structures of the response regulator DosR from
Mycobacterium tuberculosis suggest a helix rearrangement mechanism for phosphorylation activation. J Mol Biol 2008;378:227-42.



64. Park HD, Guinn KM, Harrell MI, Liao R, Voskuil MI, Tompa M, et al. Rv3133c/dosR is a transcription factor that mediates the hypoxic response of
Mycobacterium tuberculosis. Mol Microbiol 2003;48:833-43.



65. Sherman DR, Voskuil M, Schnappinger D, Liao R, Harrell MI, Schoolnik GK. Regulation of the
Mycobacterium tuberculosis hypoxic response gene encoding alpha-crystallin. Proc Natl Acad Sci U S A 2001;98:7534-9.


67. Kalscheuer R. Genetics of wax ester and triacylglycerol biosynthesis in bacteria. In: Timmis KN, editors. Handbook of hydrocarbon and lipid microbiology. Berlin: Springer; 2010. p. 527-35.
69. Sharma S, Tyagi JS.
Mycobacterium tuberculosis DevR/DosR dormancy regulator activation mechanism: dispensability of phosphorylation, cooperativity and essentiality of alpha10 helix. PLoS One 2016;11:e0160723.



70. Dasgupta N, Kapur V, Singh KK, Das TK, Sachdeva S, Jyothisri K, et al. Characterization of a two-component system, devR-devS, of
Mycobacterium tuberculosis. Tuber Lung Dis 2000;80:141-59.


71. Saini DK, Malhotra V, Dey D, Pant N, Das TK, Tyagi JS. DevR-DevS is a bona fide two-component system of
Mycobacterium tuberculosis that is hypoxia-responsive in the absence of the DNA-binding domain of DevR. Microbiology (Reading) 2004;150:865-75.


72. Perez E, Samper S, Bordas Y, Guilhot C, Gicquel B, Martin C. An essential role for phoP in
Mycobacterium tuberculosis virulence. Mol Microbiol 2001;41:179-87.


73. Hutter B, Dick T. Increased alanine dehydrogenase activity during dormancy in
Mycobacterium smegmatis. FEMS Microbiol Lett 1998;167:7-11.


74. Gonzalo-Asensio J, Mostowy S, Harders-Westerveen J, Huygen K, Hernandez-Pando R, Thole J, et al. PhoP: a missing piece in the intricate puzzle of
Mycobacterium tuberculosis virulence. PLoS One 2008;3:e3496.



75. Bretl DJ, He H, Demetriadou C, White MJ, Penoske RM, Salzman NH, et al. MprA and DosR coregulate a
Mycobacterium tuberculosis virulence operon encoding Rv1813c and Rv1812c. Infect Immun 2012;80:3018-33.



76. Pang X, Samten B, Cao G, Wang X, Tvinnereim AR, Chen XL, et al. MprAB regulates the espA operon in
Mycobacterium tuberculosis and modulates ESX-1 function and host cytokine response. J Bacteriol 2013;195:66-75.



77. Sachdeva P, Misra R, Tyagi AK, Singh Y. The sigma factors of
Mycobacterium tuberculosis : regulation of the regulators. FEBS J 2010;277:605-26.


78. He H, Hovey R, Kane J, Singh V, Zahrt TC. MprAB is a stress-responsive two-component system that directly regulates expression of sigma factors SigB and SigE in
Mycobacterium tuberculosis. J Bacteriol 2006;188:2134-43.



79. Agrawal R, Saini DK. Rv1027c-Rv1028c encode functional KdpDE two-component system in
Mycobacterium tuberculosis. Biochem Biophys Res Commun 2014;446:1172-8.


80. Heermann R, Jung K. K+ supply, osmotic stress and the KdpD/KdpE two-component system. In: Gross R, Beier D, editors. Two-component systems in bacteria. Poole: Caister Academic Press; 2012. p. 181-99.
81. Haydel SE, Clark-Curtiss JE. Global expression analysis of two-component system regulator genes during
Mycobacterium tuberculosis growth in human macrophages. FEMS Microbiol Lett 2004;236:341-7.


83. Parish T, Smith DA, Kendall S, Casali N, Bancroft GJ, Stoker NG. Deletion of two-component regulatory systems increases the virulence of
Mycobacterium tuberculosis. Infect Immun 2003;71:1134-40.



84. Bhattacharya M, Biswas A, Das AK. Interaction analysis of TcrX/Y two component system from
Mycobacterium tuberculosis. Biochimie 2010;92:263-72.


86. Haydel SE, Dunlap NE, Benjamin WH. In vitro evidence of two-component system phosphorylation between the
Mycobacterium tuberculosis TrcR/TrcS proteins. Microb Pathog 1999;26:195-206.


87. Feklistov A, Sharon BD, Darst SA, Gross CA. Bacterial sigma factors: a historical, structural, and genomic perspective. Annu Rev Microbiol 2014;68:357-76.


88. Gruber TM, Gross CA. Multiple sigma subunits and the partitioning of bacterial transcription space. Annu Rev Microbiol 2003;57:441-66.


89. Rodrigue S, Provvedi R, Jacques PE, Gaudreau L, Manganelli R. The sigma factors of
Mycobacterium tuberculosis. FEMS Microbiol Rev 2006;30:926-41.


91. Beaucher J, Rodrigue S, Jacques PE, Smith I, Brzezinski R, Gaudreau L. Novel
Mycobacterium tuberculosis anti-sigma factor antagonists control sigmaF activity by distinct mechanisms. mol microbiol 2002;45:1527-40.

92. Geiman DE, Kaushal D, Ko C, Tyagi S, Manabe YC, Schroeder BG, et al. Attenuation of late-stage disease in mice infected by the
Mycobacterium tuberculosis mutant lacking the SigF alternate sigma factor and identification of SigF-dependent genes by microarray analysis. Infect Immun 2004;72:1733-45.



93. Jeong EH, Son YM, Hah YS, Choi YJ, Lee KH, Song T, et al. RshA mimetic peptides inhibiting the transcription driven by a
Mycobacterium tuberculosis sigma factor SigH. Biochem Biophys Res Commun 2006;339:392-8.


94. Li L, Fang C, Zhuang N, Wang T, Zhang Y. Structural basis for transcription initiation by bacterial ECF sigma factors. Nat Commun 2019;10:1153.


96. Kaushal D, Schroeder BG, Tyagi S, Yoshimatsu T, Scott C, Ko C, et al. Reduced immunopathology and mortality despite tissue persistence in a
Mycobacterium tuberculosis mutant lacking alternative sigma factor, SigH. Proc Natl Acad Sci U S A 2002;99:8330-5.


97. Graham JE, Clark-Curtiss JE. Identification of
Mycobacterium tuberculosis RNAs synthesized in response to phagocytosis by human macrophages by selective capture of transcribed sequences (SCOTS). Proc Natl Acad Sci U S A 1999;96:11554-9.



99. Banaiee N, Jacobs WR Jr, Ernst JD. Regulation of
Mycobacterium tuberculosis whiB3 in the mouse lung and macrophages. Infect Immun 2006;74:6449-57.



100. Singh A, Crossman DK, Mai D, Guidry L, Voskuil MI, Renfrow MB, et al.
Mycobacterium tuberculosis WhiB3 maintains redox homeostasis by regulating virulence lipid anabolism to modulate macrophage response. PLoS Pathog 2009;5:e1000545.










 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



