Fistula Formation between Right Upper Bronchus and Bronchus Intermedius Caused by Endobronchial Tuberculosis: A Case Report
Article information
Abstract
Endobronchial tuberculosis is defined as a tuberculous infection of the tracheobronchial tree and has a prevalence of up to 50% in active pulmonary tuberculosis cases. The most common complication of endobronchial tuberculosis is bronchial stenosis; benign fistula formation by endobronchial tuberculosis is rare, especially inter-bronchial fistula formation. We reported a rare case of a 73-year-old woman with a fistula between the right upper bronchus and bronchus intermedius. A diagnosis of inter-bronchial fistula caused by endobronchial tuberculosis was based on the results of chest computed tomography scans, bronchoscopy, and microbiological and pathological tests. The patient was treated with anti-tuberculous medication, and her symptoms gradually improved.
Introduction
Endobronchial tuberculosis (EBTB) is defined as a tuberculous infection of the tracheobronchial tree with microbial and pathological evidence. EBTB is a highly infectious disease that has a prevalence of 10%-50% in patients with active pulmonary tuberculosis1.
Many patients with EBTB have some degree of complications. The most common complication is bronchial stenosis, which can become a clinical problem. Fistula formation by tuberculosis is a very rare complication and bronchopleural fistula is the most commonly observed form of fistula2. Broncho-bronchial fistula caused by tuberculosis is very rarely reported3. Herein, we report a rare case of fistula formation between the right upper bronchus and bronchus intermedius in a 73-year-old woman who presented with anorexia and general weakness.
Case Report
A 73-year-old woman presented to the emergency room with cough, anorexia, and general weakness, symptoms that had been present over a period of 2 months. The only disease found in her medical history was ischemic heart disease, which was diagnosed 4 years previously. Her vital sign and physical examinations were normal, although she presented with low-grade fever and fine inspiratory crackle in the right middle lung fields on auscultation.
Routine laboratory values were within normal limits, although the patient was anemic, with hemoglobin levels of 10.7 g/dL, and presented with hyponatremia (126 mEq/L), hypoalbuminemia (3.0 g/dL), and elevated C-reactive protein levels (12.26 mg/dL). Three acid-fast bacilli tests of sputum were negative. A chest radiograph showed an ill-defined consolidation in the right lower lung fields and fibrotic change in the right upper lung fields (Figure 1). Computed tomography (CT) scans of the chest showed multiple, ill-defined nodules in the right middle lung and multiple variable-sized mediastinal lymph nodes (Figure 2A). In addition, CT scans of the chest showed an irregular cavity that communicated from the right upper lobe bronchus to the bronchus intermedius (Figure 2B, C). These findings were compatible with an interbronchial fistula.
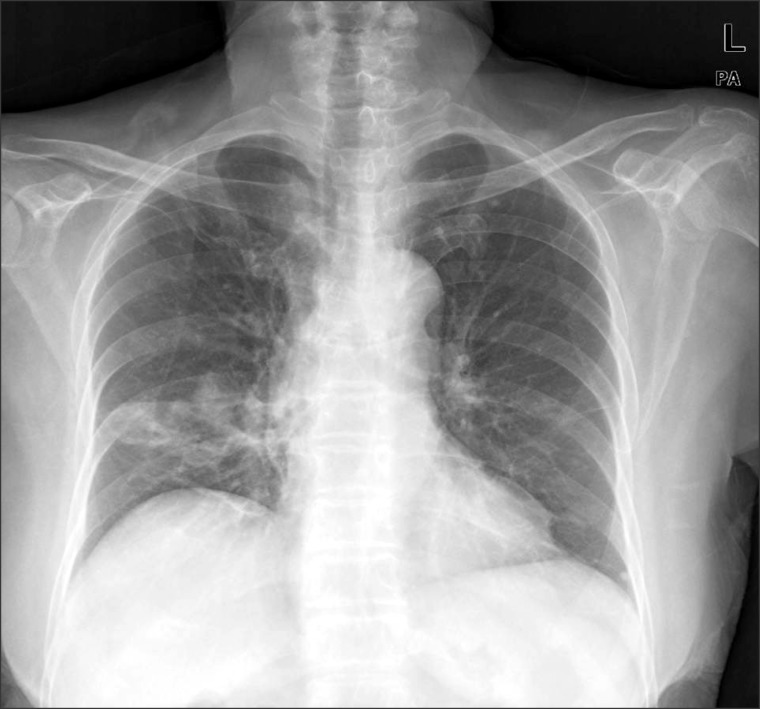
A chest radiograph revealed an ill-defined consolidation in the right lower lung fields and fibrotic change in the right upper lung fields.
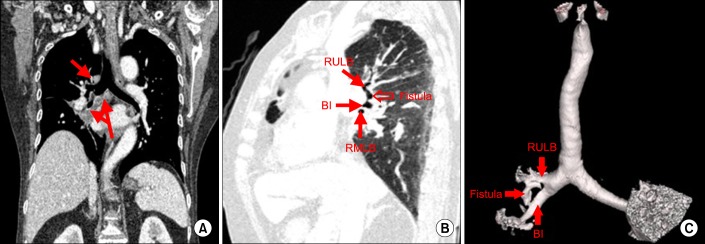
(A) Coronal image of the chest obtained using computed tomography (CT) scan revealed multiple variable-sized mediastinal lymph nodes. (B) Sagittal image of chest obtained using CT scan showed the whole pathway of the broncho-bronchial fistula, which originated in the right upper lobe bronchus and inserted in the bronchus intermedius. (C) The volume rendering image showed the presence of a fistula between the right upper lobe bronchus and the bronchus intermedius. RULB: right upper lobe bronchus; BI: bronchus intermedius; RMLB: right middle lobe bronchus.
Bronchoscopy revealed an approximately 3-mm bronchial wall defect with round and relatively well-defined margins at the anterior wall of the right upper bronchus and the lateral aspect of the distal bronchus intermedius (Figure 3). Bronchial washing and biopsy were obtained in anterior wall defect of right upper bronchus. Acid-fast bacillus stain, culture, tuberculosis polymerase chain reaction, and biopsy results were all compatible with a diagnosis of tuberculosis. Bacteria, fungal culture, and malignant cells were not observed in washing fluids or biopsy. A diagnosis of fistula formation between the right upper bronchus and bronchus intermedius caused by EBTB was made and, following the initiation of anti-tuberculosis medications, the patient's symptoms gradually improved.

(A) A round bronchial wall defect of approximately 3 mm was found at the anterior wall of the right upper lobar bronchus. (B) A round bronchial wall defect of approximately 3 mm was found at the lateral aspect of the distal bronchus intermedius. RULB: right upper lobe bronchus; RLLB: right lower lobe bronchus; RMLB: right middle lobe bronchus.
Discussion
Despite extensive global control efforts, tuberculosis remains a serious problem in developing countries. In addition, the prevalence of tuberculosis in developed countries is increasing, as a result of increased human immunodeficiency virus infections, increased immigration rates, and other failures of the general health care service4.
EBTB is defined as a tuberculosis infection in the tracheobronchial tree and it reported a prevalence of 53% in patients with active pulmonary tuberculosis1. EBTB is of clinical importance due to its high infectivity and complications. Bronchial stenosis is the most common complication of EBTB and is sometimes misdiagnosed as bronchial asthma as it can cause serious respiratory distress5.
A bronchial fistula is defined as an abnormal passage or communication between a bronchus and another part of body. It may develop when there are penetrating wounds of the thorax, following surgery, or, more rarely, as a result of granulomatous infection or malignancy of the lungs. A bronchial fistula may occur anywhere, including the esophagus, mediastinum, pleural cavity, and skin. The most commonly observed form of bronchial fistula is bronchopleural. Broncho-bronchial fistulas are very rarely reported3.
The development of a bronchial fistula in tuberculosis is related to mediastinal lymph node involvement6. Inflammation in and around enlarged lymph nodes leads to the involvement of neighboring structures or organs. In our patient, multiple, variable-sized mediastinal lymph nodes were observed and were considered to be a possible etiology.
A bronchial fistula is normally diagnosed through a combination of methods, including by CT, flexible bronchoscopy, esophagogastroscopy, and barium esophagography. However, recently a number of new novel methods have been used in the diagnosis of bronchopleural fistula7. In our case, broncho-bronchial fistula was diagnosed using three-dimensional reconstruction of the volume acquisition obtained using the spiral technique of CT and flexible bronchoscopy.
The main treatment approach for bronchial fistula caused by active tuberculous infection is the eradication of Mycobacterium tuberculosis. The next step is to prevent and treat secondary complications, such as infection. If medical treatment fails to treat fistula, secondary intervention may be needed. Traditionally, primary or delayed closure has been performed, but less invasive techniques, such as bronchoscopy assisted glue injection or coil and stent insertion, is now available to treat such lesions8.
To treat our patient, we initiated anti-tuberculosis therapy without any secondary intervention for the fistula, and her symptoms gradually improved. However, it is unknown how long medication should be used for disease control and to prevent relapse, as few cases of broncho-bronchial fistula have been reported. Additional clinical investigations of broncho-bronchial fistula is required.
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.