Correlation between Physical Activity and Lung Function in Dusty Areas: Results from the Chronic Obstructive Pulmonary Disease in Dusty Areas (CODA) Cohort
Article information
Abstract
Background
Although physical activity is known to be beneficial to lung function, few studies have been conducted to investigate the correlation between physical activity and lung function in dusty areas. Therefore, the purpose of this study is to investigate the correlation between physical activity and lung function in a Korean cohort including normal and COPD-diagnosed participants.
Methods
Data obtained from the COPD in dusty areas (CODA) cohort was analyzed for the following factors: lung function, symptoms, and information about physical activity. Information on physical activity was valuated using questionnaires, and participants were categorized into two groups: active and inactive. The evaluation of the mean lung function, modified Medical Research Council dyspnea grade scores, and COPD assessment test scores was done based on the participant physical activity using a general linear model after adjusting for age, sex, smoking status, pack-years, height, and weight. In addition, a stratification analysis was performed based on the smoking status and COPD.
Results
Physical activity had a correlation with high forced expiratory volume in 1 second (FEV1) among CODA cohort (p=0.03). While the active group exhibited significantly higher FEV1 compared to one exhibited by the inactive group among past smokers (p=0.02), no such correlation existed among current smokers. There was no significant difference observed in lung function after it was stratified by COPD.
Conclusion
This study established a positive correlation between regular physical activity in dusty areas and lung function in participants.
Introduction
World Health Organization (WHO) has reported that 65 million people have a moderate-to-severe chronic obstructive pulmonary disease (COPD) and that COPD will become the third leading cause of death worldwide by 20301. COPD is reportedly characterized by both low lung function and accelerated decline in lung function2. With aging, lung function and respiratory muscle strength decrease3, and most patients with COPD are not diagnosed accurately4. Although smoking is a well-known risk factor5, environmental factors, such as air pollution and occupational exposure, are also crucial risk factors for COPD6. Furthermore, exposure to cement dust is correlated with a higher prevalence of COPD and respiratory symptoms7.
WHO recommends exercise training programs for managing COPD8. Physical activity reduces all-cause cardiovascular and respiratory mortality risk and exacerbation910. In addition, physical activity has been associated with high lung function in European study11. The beneficial effects of physical activity have been reported not only in patients with COPD but also in healthy adults and children1213. Considering environmental pollution and lung health, it is unclear whether exposure to air pollution during physical activity affects the beneficial effects of physical activity. A previous study has reported that air pollution did not affect the beneficial effects of physical activity on reducing the risk of COPD14. Furthermore, physical activity positively affected lung function when performed in a highly polluted environment15. Studies on physical activity and lung function during air pollution exposure have been reported; however, studies on specific environmental exposures, such as cement dust, are limited.
The COPD in dusty areas (CODA) cohort study collected epidemiological and clinical data from participants living near cement plants where cement dust affected them16. This study aimed to assess the correlation between physical activity and lung function using the CODA study data to assess the effect of physical activity on lung function a Korean cohort including normal and COPD-diagnosed participants in dusty areas.
Materials and Methods
1. Study design and population
Data from the CODA study were analyzed. The objectives and design of the CODA study have been detailed elsewhere17. Briefly, the CODA study enrolled participants living in six areas near cement plants in the Kangwon and Chungbuk provinces of South Korea. Overall, 504 participants (362 males and 142 females) were enrolled between 2012 and 2017 for baseline examinations.
At baseline examinations, data on the medical interview, survey questionnaire, spirometry, physical examination, blood/urine samples, and computed tomography were obtained from all participants. Questionnaire data included demographic factors, lifestyle factors, history of the disease, history of exacerbation, and symptoms of participants during the past year. Among the 504 participants, five with no information on physical activity were excluded from the analysis. Finally, we analyzed 499 participants. Written informed consent was given by each participants. This study received ethical approval from the Kangwon National University Hospital IRB (KNUH 2012-06-007).
2. Measurement
We performed spirometry using an Easy One Kit (NDD, Zurich, Switzerland). All lung function tests were performed as recommended by the American Thoracic Society/European Respiratory Society18. We defined COPD as post-bronchodilator forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) ratio of <0.7. We assessed physical activity using questionnaires. Participants reported whether they performed regular physical activities until they sweated during the past year (yes/no); accordingly, we categorized the participants into activity and inactivity groups.
In this study, the following demographic and lifestyle factors were included: age, sex, education, marriage status, income, smoking status, and pack-years of cigarette smoking. Dyspnea was assessed using the modified Medical Research Council (mMRC) dyspnea grade. We evaluated health-related quality of life by calculating the total score on the patient-reported COPD Assessment Test (CAT).
3. Statistical analysis
Continuous variables were presented as mean±standard deviation, and categorical variables were presented as frequencies and percentages. The least square means of the lung function, mMRC scores, and CAT scores based on physical activity were evaluated using a general linear model. The mean of lung function was adjusted for age, sex, smoking status, pack-years of cigarette smoking, and height, whereas the means of the mMRC and CAT scores were adjusted for age, sex, smoking status, and pack-years of cigarette smoking. Furthermore, we performed a stratification analysis for smoking status, COPD, and COPD severity. For classification of COPD severity among COPD patients, we classified as follows: mild, FEV1≥80% predicted; moderate, 50%≤FEV1<80% predicted; and ≥severe, FEV1<50% predicted19.
In this study, all statistical analyses were performed using SAS (version 9.4, SAS Institute Inc., Cary, NC, USA). We considered statistical significance at p<0.05.
Results
Table 1 summarizes the baseline characteristics of the participants. The mean age of the participants was 72 years, and 72% were male. While 43% were former smokers, 20% were current smokers. In addition, the mean pack-year of cigarette smoking of the participants was 17, and the pack-years of cigarette smoking was higher in the inactivity group than the activity group.
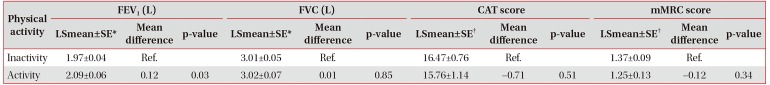
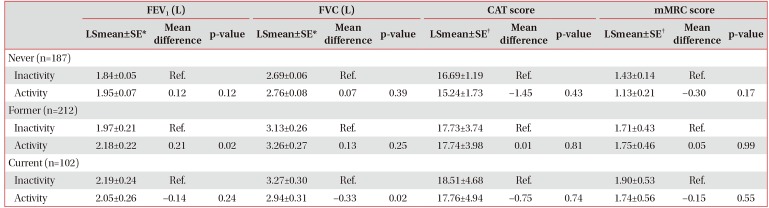
Table 2 presents the correlation between lung function and symptoms based on physical activity at baseline. Compared with inactivity group, the mean FEV1 adjusted for confounding factors was higher in the activity group. The mean FEV1 was 1.97 and 2.09 L among inactive and active participants, respectively (p=0.03). However, no significant difference in the FVC, CAT scores, and mMRC scores was observed. In the stratification analysis by smoking status, the activity group exhibited higher FEV1 than that exhibited by the inactivity group among former smokers. The mean FEV1 of inactive and active participants was 1.97 and 2.18 L, respectively (p=0.02). The activity group exhibited lower FVC than that exhibited by the inactivity group among current smokers. The mean FVC of inactive and active participants was 3.27 and 2.94 L, respectively (p=0.02) (Table 3). We observed no significant difference in the stratification analysis by COPD (Table 4). As a result of stratification analysis by COPD severity, the activity group exhibited a higher FEV1 than the inactivity group in mild COPD subgroup (Table 5).

Correlation between the lung function and symptoms and physical activity at the baseline by the smoking status
Discussion
This study established a correlation between physical activity and FEV1 in elderly participants from the CODA cohort study. After adjusting for confounding factors, the activity group exhibited higher FEV1 than that exhibited by the inactivity group. This correlation was observed among former smokers; however, no such correlation was observed in the stratification analysis by COPD.
Among all the participants, only 23% performed regular physical activity. In Korea, cement plants are located in the rural areas of Kangwon and Chungbuk that have a relatively more aged population. The Korea National Health and Nutrition Examination Survey reported that the percentage of aerobic and muscular physical activity in adults aged >65 years was 34.4% and 15.2%, respectively20. In this study, the questionnaire focused on regular physical activities until participants sweated. Only a small proportion in this cohort answered this question affirmatively, perhaps because our study cohort represented a more aged population.
This study corroborates the findings of two prior studies on older adults. In the European Prospective Investigation of Cancer (EPIC)-Norfolk study, FEV1 was higher with escalating vigorous activity time in adults aged 45–74 years21. The English Longitudinal Study of Aging reported a positive correlation between physical activity and lung function in adults with an average age of 63 years22. In COPD, which is characterized by low lung function, the quality of life could be decreased because of exacerbation, hospitalization, and mortality23, which can be reduced due to physical activity2425. In addition, Esteban et al. have reported that among older patients with COPD, those with high levels of physical activity had enhanced health-related quality of life26. Despite being insignificant in the COPD subgroup, the current study demonstrated a positive effect of physical activity on lung function in all cohort participants. Of note, a negative result of the subgroup could be attributed to the relatively small sample size. In previous study from elderly COPD patients in Korea, increased dyspnea scale and presence of depression were associated with low-level physical activity27.
Reportedly, smoking reduces lung function and cardiorespiratory fitness2829. Walters et al.30 have suggested that smoking accelerates the aging of small airway epithelium at molecular levels. Hence, the stratification analysis by smoking status in this study revealed that regular physical activity correlated with high FEV1 in former smokers. Prior studies have reported inconsistent results regarding the correlation between physical activity and lung function according to smoking status. Luzak et al.13 have established a positive correlation between physical activity and lung function among ex-/current smokers, whereas Barboza et al.31 have reported no such correlation in smokers. In smokers, low-grade systemic inflammatory responses, including C-reactive protein, fibrinogen, interleukin-6, and white blood cells, have been identified, and most have recovered after smoking cessation. Nevertheless, several systemic inflammation markers increased in former smokers after they stopped smoking32. A study of adults aged >40 years indicated interactions of smoking and FEV1 on markers of systemic inflammation33. In several studies, the mechanism between physical activity and inflammatory biomarkers remains unclear, although it has been reported that physical activity correlates with low inflammatory biomarkers in elderly adults343536. The present study has reported the positive association between lung function and physical activity in former smokers. In current smokers, these beneficial effects were not observed probably because the smoking effects were very strong. The activity group had higher FEV1 than inactivity group among mild COPD subgroup. There remain inconsistent reports in beneficial effects of physical activity on quality of life, dyspnea, or long-term disease progression in patients with mild or moderate stage37.
Our study participants lived near cement plants and were exposed to cement dust. To the best of our knowledge, very few cohort studies have investigated such specific environments. Thus, a strength of this study is the acquisition of valuable and useful data. However, this study had some limitations. First, physical activity may have been underestimated because it was assessed using questionnaires. Therefore, future studies with precise assessment of physical activity are warranted. Second, this study fails to explain the causal relationship between physical activity and lung function owing to its cross-sectional study design, necessitating future analyses with longitudinal changes in lung function.
In conclusion, this study reveals that regular physical activity correlates with FEV1 in the CODA cohort, and this correlation is most robust in former smokers. Future study will be needed to evaluate the effect of regular activity on lung function in dusty areas.
Acknowledgments
We thank Seul-Kee Kim for technical support.
Notes
Authors' Contributions:
Conceptualization: Han Y, Kim WJ.
Methodology: Kwon SO, Kim WJ.
Formal Analysis: Han Y.
Data curation: Heo Y, Hong Y.
Writing - original draft preparation: Han Y.
Writing - review and editing: Heo Y, Hong Y, Kwon SO, Kim WJ.
Approval of final manuscript: all authors.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
Funding: This study was supported by 2017 Research Grant from Kangwon National University (No. 520170447) and Ministry of Environment.