Experiences of Latent Tuberculosis Infection Treatment for the North Korean Refugees
Article information
Abstract
Background
Tuberculosis (TB) is increasing in immigrants. We aimed to investigate the current status of latent tuberculosis infection (LTBI) treatment for North Korean Refugees (NKR) compared to South Koreans Contacts (SKC).
Methods
TB close contacts in a closed facility of SKC and NKR who underwent LTBI screening in a settlement support center for NKR were analyzed retrospectively.
Results
Among tuberculin skin test (TST) ≥10 mm (n=298) reactors, the males accounted for 72.2% in SKC (n=126) and 19.5% in NKR (n=172) (p<0.01). The mean age was higher in South Korea (42.8±9.9 years vs. 35.4±10.0 years, p<0.01). Additionally, the mean TST size was significantly bigger in NKR (17.39±3.9 mm vs. 16.57±4.2 mm, p=0.03). The LTBI treatments were initiated for all screened NKR, and LTBI completion rate was only 68.0%. However, in NKR, LTBI treatment completion rate was significantly increased by shorter 4R regimen (odds ratio [OR], 9.296; 95% confidence interval [CI], 4.159–20.774; p<0.01) and male (OR, 3.447; 95% CI, 1.191–9.974; p=0.02).
Conclusion
LTBI treatment compliance must be improved in NKR with a shorter regimen. In addition, a larger study regarding a focus on LTBI with easy access to related data for NKR should be conducted.
Introduction
Tuberculosis (TB) is known to be the leading cause of death among infectious diseases worldwide. However, TB incidence in South Korea (SK) has been continuously decreased to 65.9/100,000 population in 20181. Recently, latent TB infection (LTBI) treatment with political commitment accompanied by promotion of human rights has been addressed by World Health Organization2 as the END TB strategy to prevent the development of TB cases.
The percentage of immigrant TB in SK is 5.3 % in 20181. TB cases in immigrants are increasing every year345. Moreover, many refugees from North Korea (NK) where TB incidence is as high as 513/100,000 population and drug maintenance system is infirm are emigrating to SK every year67. Korean Government is screening both TB and LTBI for North Korean Refugees (NKR) from the immigration process in National Intelligence Service for security3.
For LTBI diagnosis, additional confirmatory QuantiFERON-TB Gold In Tube (QFT-GIT) test as a two-step strategy had been used for TB contacts with 10≤tuberculin skin test (TST) induration<15 mm with bacillus Calmette–Guérin (BCG) scar or identified BCG vaccination in SK89. For LTBI treatment of immigrants, the adequacy based on TB incidence rate and drug resistance rate of emigration country must be weighed against the benefit of LTBI treatment10. In case of vulnerable NKR, drug compliance and inaccessibility to health center owing to political and cultural barrier seem to be crucial11 for LTBI control policy. However, there are no reports about LTBI treatment results including optimal drug regimen for NKR, even though rifampicin containing regimen supposed to be potent as well considering its efficacy and drug compliance1213.
The purpose of this study was to compare the status of LTBI treatment between NKR and South Korean Contacts (SKC), and to investigate factors affecting drug compliance for LTBI treatment in NKR.
Materials and Methods
1. Study population
Limited LTBI screening data of NKR in 2008 when LTBI treatment program was consulted by Korean Institute of Tuberculosis were selected. As comparative data, data of TB contacts investigated in closed correctional facility of SK where consecutive active TB developed in 2007 were reviewed1415. In the NKR group, in perspective of LTBI treatment, data of TST positive reactors were only available. TST negative results (TST <10 mm) in SKC group were excluded for comparison. As a result, a total of 126 SK facility inmates and 172 NKR were retrospectively reviewed and compared. Written informed consent was obtained, and this study was approved by the Institutional Review Board (IRB) of Korean Institute of Tuberculosis (IRB number: KIT-2007-01/2009-04).
2. Policy of TB and LTBI screening for NKR
Basic health screenings including TB and LTBI are initially conducted in National Intelligence Service of SK after immigration. Although TST and confirmatory QFT-GIT had been used (two step strategy) for LTBI diagnosis in the past, recently single QFT-GIT method is being used after excluding active TB using chest radiograph (CXR) and sputum acid fast bacilli smear and culture. Initiated LTBI treatment or TB treatment for 1–2 months is continued at Hana-medical office in settlement support center (Hanawon) for NKR where 3 months' detention and education program is given. Their overlong further medical treatments are referred to near assigned hospital after their new home settlement7.
3. LTBI diagnosis
TST and additional QFT-GIT (Cellestis, Ltd, Carnegie, Australia) tests were performed as a screening test for LTBI after exclusion of active TB based on CXR in SKC and NKR groups, respectively. A TST was performed using the Mantoux method (Statens Serum Institute [SSI], Copenhagen, Denmark). The induration size was measured after 48–72 hours by experienced nurses. An induration size with TST ≥10 mm was set as cut-off value. Additional QFT-GIT tests were performed for TST positive reactors while measuring the induration size of TST. Interpretation of QFT-GIT tests followed the manufacturer's instructions16.
4. LTBI treatment
LTBI treatment was recommended for subjects with positive results of additional confirmative QFT-GIT results among TST positive reactors in both groups. But some subjects received LTBI treatment irrespective of QFT-GIT results, if they wanted to receive LTBI treatment. As LTBI treatment regimens, 4 months of rifampicin (4R) was used in SKC and 9 months of isoniazid (9H) or 4R were prescribed to individuals of the NKR after consultations to a charge doctor in Korean Institute of Tuberculosis. LTBI treatment and adverse drug reaction was monitored for both groups. LTBI treatment completion was defined as finishing ≥80% of the prescribed pills.
5. Statistical analysis
All analyses were performed using SPSS software version 20.0 (IBM Corp., Armonk, NY, USA). Chi-square test and Mann-Whitney test after checking normal distribution of data were used. All tests for significance were two-sided. Statistical significance was set at p<0.05. Associations of LTBI treatment completion with group, drug regimen, adverse drug reaction, sex, and age were analyzed by binary logistic regression.
Results
1. Clinical characteristics
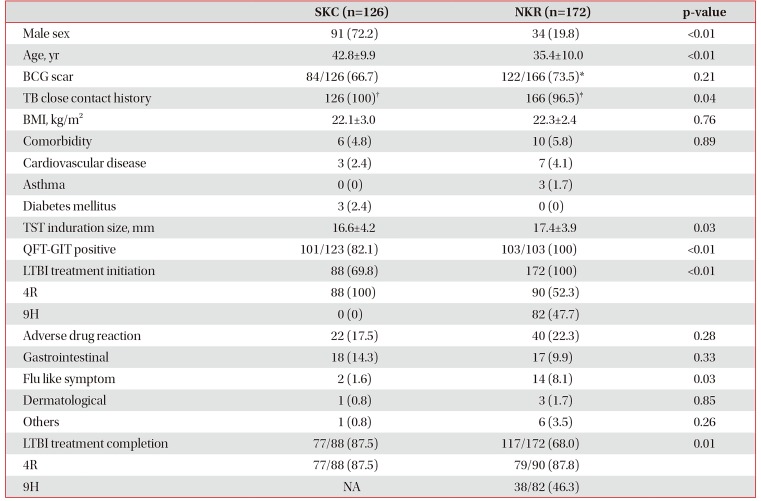
A total of 126 SK facility inmates who were investigated after TB outbreaks and 172 NKR who underwent immigrants TB screening were enrolled for this study. These characteris are summarized in Table 1. The ratio of male was higher in SKC (p<0.01). Mean age was higher in SKC than in NKR (p<0.01). BCG scar rate was not significantly different between the two groups (p>0.05). TB close contact histories from families existed in NKR (96.5%) whereas SKC had contact histories to an index infectious TB case (100%). Comorbidity conditions were not significantly different between the two groups (p>0.05). Mean body mass index was not significantly different between the two groups either (p>0.05) (Table 1).
2. Diagnosis and treatment of LTBI
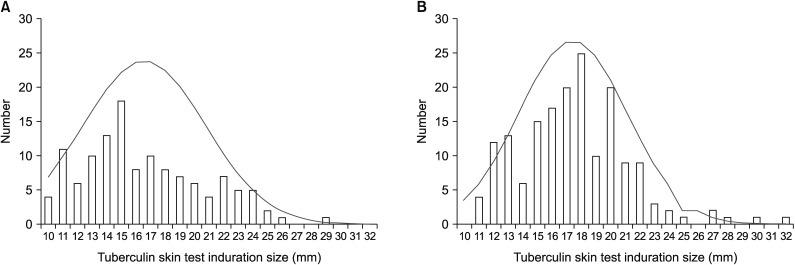
As shown in Figure 1, the distribution of TST positive reactors were right shifted in NKR compared with SKC. The induration size of TST was 16.6±4.2 mm in SKC (A) and 17.4±3.9 mm in NKR (B) with significant difference (p=0.03). The QFT-GIT positive rate was 82.1% in SKC and 100% in NKR. LTBI treatment in SKC was initiated for 88 patients (69.8%), all of whom were prescribed 4R. In NKR, 172 (100%) people received LTBI treatment initially, of which 52.3% were prescribed 4R while the remaining 47.7% were prescribed 9H. LTBI treatment completion rate was significantly higher in SKC (77/88, 87.5%) than that in NKR (117/172, 68.0%). Among NKR, LTBI completion rate was 87.8% in 4R and 46.3% in 9H, respectively. However, the overall frequency of adverse drug reaction was not different between two groups (Table 1). During 2 years of follow-up after LTBI treatment, one active TB developed in SKC, but none in NKR.
3. Factors associated with LTBI treatment completion
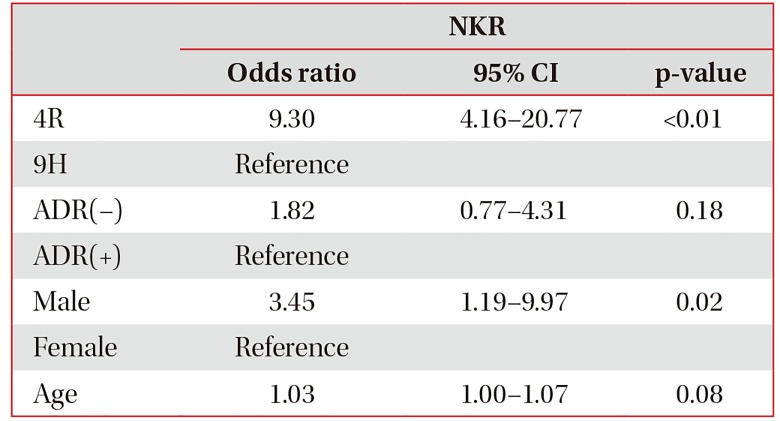
When LTBI treatment completion rate was analyzed in NKR as a binary logistic regression, 4R regimen (odds ratio [OR], 9.30; 95% confidence interval [CI], 4.16–20.77; p<0.01) and male sex (OR, 3.45; 95% CI, 1.19–9.97; p=0.02) significantly contributed to the increased LTBI completion rate in NKR after adjusting for other variables, although age showed borderline statistical significance (OR, 1.03; 95% CI, 1.00–1.07; p=0.08) (Table 2).
Discussion
As a LTBI treatment regimen for NKR, 4R regimen with shorter period showed higher completion rate than 9H. However, larger study including other regimen with long-term follow-up must be conducted for NKR.
As shown in Figure 1, distribution of TST for positive results in NKR was shifted to the right than that in SKC where older ages were distributed. Although NKR were not proven TB close contacts in a TB outbreak setting as in SKC where exposure time to an active TB index case was very long in a closed correctional facility, casual TB contacts in NKR were supposed to have been frequent and extensive in ordinary life17. In addition, considering high QFT-GIT positive rate among TST reactors (TST ≥10 mm) (100%, 103/103), further study about the role of additional QFT-GIT in relation with TST size must be elucidated.
The initiation rate for LTBI treatment was much higher in NKR than that in SKC. This was because NKR were protected and managed by a governmental isolated secret facility (Hanawon) medically and politically in the initial settlement period18. However, the overall rate of LTBI treatment completion in NKR was not high because LTBI completion had been dependent on sex and drug regimen, not on adverse drug reactions. Low completion rate in 9H can be originated from the lesser attention after home settlement out of Hanawon.
Based on our results, special attention is needed for female NKR on LTBI treatment completion, and shorter regimen including rifampicin regimen such as 4R or 3HR should be recommend for NKR for better compliacne1920, considering isoniazid abuse in the underground market, “Jangmadang” in NK21. And if possible, Directly Observed Treatment, in short course in Hanawon should be performed to increase compliance.
This study has several limitations. First, data of TB contacts with <TST 10 mm could not be collected or analyzed because access to data of NKR was limited. Second, TB exposure setting was not well defined for NKR, and exposure time to family active TB cases for NKR could not be identified. Lastly, the enrolled number was too small to represent all people of NKR. In conclusion, for NKR, 4R regiment instead of 9H should be considered as a LTBI treatment regimen. Further larger study about LTBI for NKR should be conducted with easy access to related data for NKR.
Notes
Authors' Contributions:
Conceptualization: Kim HJ (for Hee Jin Kim), Lee SH.
Methodology: Cha JH, Kim HJ (for Hee Jin Kim), Lee SH.
Formal analysis: Kim BK, Cha JH, Kim CY, Kim Y, Lee SH.
Investigation: Kim HJ (for Hee Jin Kim), Kim HJ (for Ho Jin Kim), Lee JB, Jeon J, Lee SH.
Writting - original draft preparation: Kim BK, Kim HJ (for Ho Jin Kim), Kim HJ (for Hee Jin Kim), Lee SH.
Writing - review and editing: Kim BK, Kim HJ (for Hee Jin Kim), Kim Y, Kim JH, Shin C, Lee SH.
Approval of final manuscript: all authors.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
Funding: No funding to declare.