Risk Factors for Predicting Hypoxia in Adult Patients Undergoing Bronchoscopy under Sedation
Article information
Abstract
Background
Flexible bronchoscopy is one of the essential procedures for the diagnosis and treatment of pulmonary diseases. The purpose of this study was to identify the risk factors associated with the occurrence of hypoxia in adults undergoing flexible bronchoscopy under sedation.
Methods
We retrospectively analyzed 2,520 patients who underwent flexible bronchoscopy under sedation at our tertiary care university hospital in South Korea January 1, 2013–December 31, 2014. Hypoxia was defined as more than 5%-point reduction in the baseline percutaneous oxygen saturation (SpO2) or SpO2 <90% for >1 minute during the procedure.
Results
The mean age was 64.7±13.5, and 565 patients developed hypoxia during the procedure. The mean sedation duration and midazolam dose for sedation were 31.1 minutes and 3.9 mg, respectively. The bivariate analysis showed that older age, a low forced expiratory volume in one second (FEV1), use of endobronchial ultrasound, the duration of sedation, and the midazolam dose were associated with the occurrence of hypoxia during the procedure, while the multivariate analysis found that age >60 (odds ratio [OR], 1.32), a low FEV1 (OR, 0.99), and a longer duration of sedation (>40 minutes; OR, 1.33) were significant risk factors.
Conclusion
The findings suggest that patients older than age 60 and those with a low FEV1 tend to develop hypoxia during the bronchoscopy under sedation. Also, longer duration of sedation (>40 minutes) was a significant risk factor for hypoxia.
Introduction
Flexible bronchoscopy is one of the most important procedures for diagnosis and treatment of pulmonary disease [1]. Bronchoscopy is also essential for mediastinal lymph node examination during nodal staging in patients with lung cancer [2-5]. For better patient tolerance, bronchoscopists can choose to perform the procedure under sedation [6,7]. However, bronchoscopy under sedation is not easily performed in many hospitals because of the risk of several complications [1,8], even though bronchoscopy itself is generally considered a safe procedure [9]. Complications of bronchoscopy include bleeding, pneumothorax, fever, infection, and cardiac arrhythmia [10-12]. Although oxygen supplementation is routinely provided, hypoxia is a frequent event during bronchoscopy, particularly when sedation is used [13-15]. It is generally transient and resolves instantly; however, the clinician should consider terminating the procedure in cases where hypoxia persists for >1 minute [1]. Several studies have reported the risk factors associated with hypoxia during bronchoscopy for foreign body removal in children [16,17]. The findings of those studies indicated that the patient’s age and procedure duration were associated with the occurrence of hypoxia during bronchoscopy [16,17]. However, few studies have reported the risk factors for predicting hypoxia in elderly patients undergoing bronchoscopy under sedation. Accordingly, the aim of this study was to identify the risk factors associated with hypoxia during flexible bronchoscopy under sedation in adult patients.
Materials and Methods
1. Study design
We retrospectively analyzed 3,508 patients aged >19 years who underwent flexible bronchoscopy under sedation at our tertiary care university hospital in South Korea between January 1, 2013 and December 31, 2014. Patients who underwent bronchoscopy without sedation (n=451) or with intubation (n=537) were excluded (Figure 1).
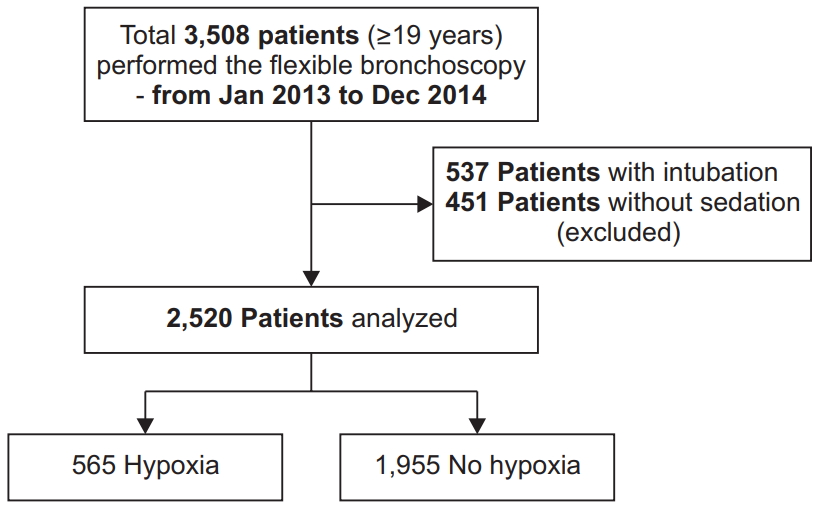
Flow chart of the inclusion and the exclusion procedures for the study. A total of 3,508 patients were enrolled, and 2,520 were included in the analysis.
We collected all relevant data associated with bronchoscopy under sedation, including baseline characteristics, pulmonary function test (PFT) results, echocardiography findings, and chest computed tomography (CT) findings just before the procedure in order to evaluate their associations with the occurrence of hypoxia during the procedure. Several factors associated with the bronchoscopy procedure, including the type of procedure, durations of the procedure and sedation, doses of sedative drugs (midazolam and fentanyl), and diameter of the bronchoscope, were also reviewed. The institutional review board (IRB 4-2019-0274) of Severance Hospital approved this retrospective study and waived the need for informed consent.
2. Procedure and sedation
Bronchoscopy was performed under topical and intravenous anesthesia with spontaneous breathing. Before the procedure, 4% lidocaine spray was applied in the oral cavity for topical anesthesia. Sedative drugs, including midazolam (0.03–0.05 mg/kg) and 50 µg of fentanyl, were administered just before the procedure at the discretion of the bronchoscopist. With the patient in the supine position, the bronchoscope was inserted through the oral or nasal cavity depending on the patient’s condition. Then, 4% lidocaine was applied to the vocal cords, main carina, and both main bronchi through a channel of the bronchoscope. The target level of sedation was moderate so that patients could purposefully respond to verbal commands while maintaining a functional airway and cardiovascular function. The bronchoscopist used additional midazolam or fentanyl doses to maintain the level of sedation during the procedure.
Hypoxia was defined as more than 5%-point reduction in the baseline percutaneous oxygen saturation (SpO2) or SpO2 <90% for >1 minute during the procedure. The oxygen of 4 L/min was applied through a nasal cannula to all patients before the bronchoscopy was started, and oxygen supplement was increased to 8 L/min in case of desaturation. If oxygen desaturation was not recovered despite maximal oxygen support, the procedure was stopped according to the decisions of bronchoscopist. Electrocardiograms and vital signs, including blood pressure, heart rate, and oxygen saturation, were continuously monitored during the procedure.
3. Statistical analysis
All data were statistically analyzed using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). Categorical variables are presented as numbers with percentages and were analyzed using the chi-squared test. Continuous variables are presented as means±standard deviations and were evaluated using Student’s t-test. Multivariate logistic regression analysis was used to evaluate the association between risk factors and the development of hypoxia during the procedure, with the results presented as odds ratios (ORs) with 95% confidence intervals (CIs). A p-value of <0.05 was considered statistically significant.
Results
1. Baseline characteristics of the study population
The study sample comprised of 1,585 men (62.9%) and 935 women (37.1%). A total of 1,654 (65.6%) patients were >60 years old, with a mean age of 64.7±13.5 years. With regard to the smoking status, 1,178 patients (46.7%) were never-smokers and 1,342 (53.2%) were ever-smokers. The most common underlying disease was hypertension (36.7%).
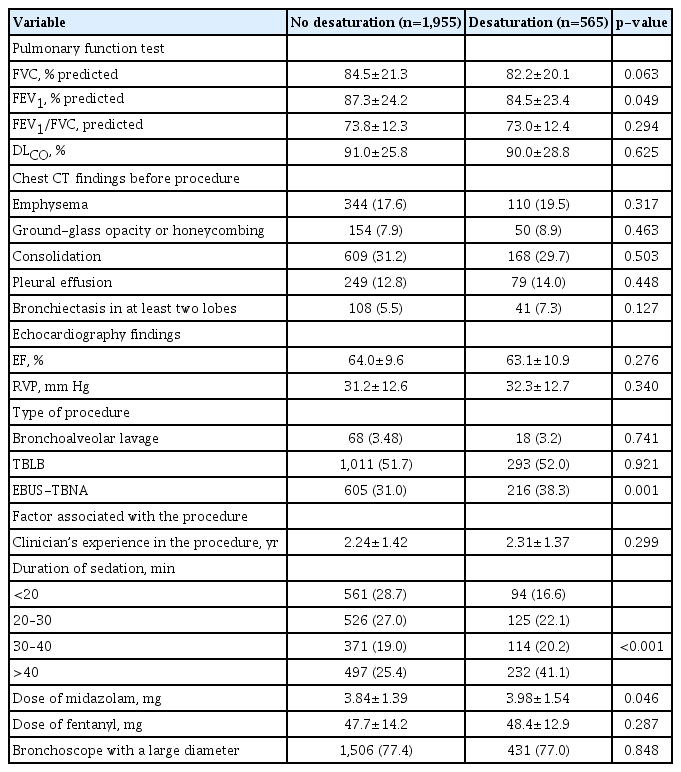
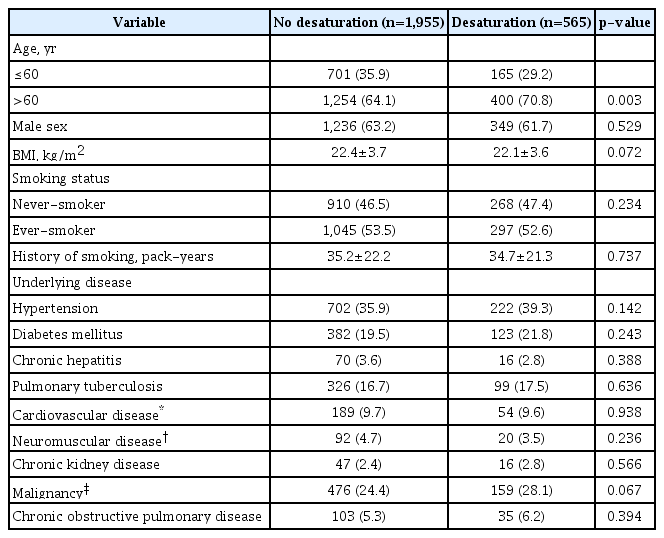
Tables 1 and 2 show the baseline characteristics of patients according to the occurrence of hypoxia during bronchoscopy under sedation. In total, 565 of the 2,520 patients (22.4%) developed hypoxia. The initial saturation level was not different between the two groups. The proportion of patients aged >60 years was significantly higher in the desaturation group than in the no desaturation groups (p=0.003). There were no between-group differences in terms of sex, the smoking status, the history of smoking (pack-years), and prevalence of underlying diseases. Patients with hypoxia presented a significantly lower forced expiratory volume in 1 second (FEV1) just before the procedure (p=0.049) (Table 2). However, the forced vital capacity (FVC), FEV1/FVC ratio, and diffusing capacity of the lung for carbon monoxide (DLCO) were comparable between groups. Finally, there were no significant between-group differences in terms of chest CT and echocardiography findings.
Baseline characteristics of patients stratified according to the occurrence of desaturation during flexible bronchoscopy under sedation
2. Procedural factors associated with hypoxia development
In total, 86 patients (3.4%) underwent bronchoscopy with bronchoalveolar lavage (BAL), while 1,304 (51.7%) and 821 (32.6%) patients underwent transbronchial lung biopsy and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA). The mean duration of sedation and mean dose of midazolam for sedation were 31.1±17.3 minurwa and 3.9±2.4 mg. Table 2 shows the factors associated with bronchoscopy according to the occurrence of hypoxia during the procedure. The proportion of patients who underwent EBUS-TBNA was significantly higher in the desaturation group than in the no desaturation group (p=0.001). There were no significant between-group differences for the other procedures. Moreover, the duration of sedation was significantly longer (p<0.001) while the midazolam dose was significantly higher (p=0.046) in the desaturation group than in the no desaturation group. There were no between-group differences in terms of the fentanyl dose, procedure duration, and use of a bronchoscope with a large diameter.
We performed multivariate analysis to analyze factors that were significant in bivariate analysis, including age >60 years, low FEV1 in PFT, use of EBUS-TBNA, duration of sedation, and midazolam dose (Table 3). Age >60 years (OR, 1.32; 95% CI, 1.007–1.734), a low FEV1 in PFT (OR, 0.99; 95% CI, 0.989–0.999), and a longer duration of sedation (>40 minutes; OR, 1.33; 95% CI, 1.179–1.499) were significantly associated with the occurrence of hypoxia.
Discussion
The results of this study showed that an age of >60 years, a low FEV1, and a longer duration of sedation were significant predictors of the occurrence of hypoxia during bronchoscopy under sedation in adults.
Flexible bronchoscopy is an essential diagnostic and therapeutic procedure in respiratory medicine. However, it leads to coughing and discomfort in patients [1]. Sedation is used for not only surgery but also various other procedures [8,18]. Several patients are more comfortable undergoing endoscopy under sedation; therefore, gastrointestinal endoscopy is commonly performed under sedation [19-21]. In addition, there have been efforts to perform bronchoscopy under sedation, which is reportedly associated with increased patient and clinician satisfaction [6,22]. Thus, bronchoscopy under sedation is generally recommended in the absence of any contraindications [1,23].
However, several centers still do not use sedation during bronchoscopy because of the risk of side effects. Complications of bronchoscopy include bleeding, pneumothorax, fever, hypoxia, and cardiac arrhythmia [10-12], and hypoxia is a common event during bronchoscopy under sedation. In most cases, it is transient and resolves quickly [24-26], although the bronchoscopist may need to stop the examination and increase the oxygen supply or wake the patient during the procedure. If the hypoxia does not resolve, the procedure should be terminated [27]. A previous study reported that bronchoscopy under sedation provides comfort to the patient and bronchoscopist [28], while other studies evaluated drugs that are more effective for sedation during the procedure [29,30]. However, few studies have analyzed the risk factors for hypoxia during bronchoscopy under sedation in adults [15,31], although some have analyzed these risk factors for pediatric patients undergoing foreign body removal via bronchoscopy [16,17]. Determination of these risk factors for adult patients is important because of the widespread use of bronchoscopy, including interventional bronchoscopy [7], and the increase in the number of elderly patients undergoing the procedure [32].
Silvestri et al. [33] evaluated the use of fospropofol disodium for sedation in patients undergoing flexible bronchoscopy and reported that hypoxia was more frequent in older patients than in younger patients, although the difference was not significant. In the present study, an age of >60 years was found to be significantly associated with the occurrence of hypoxia during bronchoscopy under sedation. Another significant risk factor was a low FEV1. Jones and O’Driscoll [24] also reported that the risk of desaturation during bronchoscopy was higher for patients with a lower FEV1, suggesting that those patients required oxygen supplementation during the procedure. Finally, Chen et al. [17] reported that the longer duration of surgical procedure (>20 minutes) was correlated with intraoperative hypoxemia in young patients undergoing rigid bronchoscopy. And, Bittencourt et al. [16] had also resulted that a longer procedure time was vulnerable to a risk of hypoxemia in children. In our study result, we found that a longer duration of sedation (>40 minutes) was a significant risk factor for hypoxia.
In previous studies, bronchoscopy with BAL was related to the occurrence of hypoxia during the procedure [34,35]. This association was not observed in the present study, probably because only 3.4% patients underwent bronchoscopy with BAL. Therefore, additional studies in a larger number of patients are necessary to evaluate the association between bronchoscopy with BAL and hypoxia. Furthermore, there are several studies related to the risk of hypoxia during bronchoscopy in patients with severe chronic lung disease and heart failure [36,37]. However, in our study, there were no association between development of hypoxia and prevalence of underlying disease or results of chest CT and echocardiography. We only investigated the presence of underlying disease, so we could not reflect the severity of that disease. Therefore, further research about the risk of hypoxia during bronchoscopy with sedation according to the severity of the disease is needed.
Our study has several limitations. First was the retrospective, single-center design. Second, subjective symptoms that can affect the occurrence of hypoxia, such as dyspnea, cough, and sputum, were not investigated. Third, although we investigated the total sedation time, the actual procedure duration was difficult to record because our analysis was retrospective. Fourth, we could not investigate the history of obstructive sleep apnea (OSA), although patients with OSA might be vulnerable to develop hypoxia during procedure with sedation. Fifth, there is a statistically significant difference between FEV1% predicted and occurrence of hypoxia in our study. But the actual difference of is only 3% (87.3 vs. 84.5) between two groups. Most of the patients included in our study had normal lung function, and patients with less than 50% of predictive FEV1 values were only 4.8% of all patients. For this reason, these differences could not have clinically valuable meaning.
Nevertheless, this study also has its strengths. Our results were obtained for a large number of patients and can be used to predict the occurrence of hypoxia during bronchoscopy under sedation before the procedure. Thus, the bronchoscopist can evaluate the risk of hypoxia in advance and prepare any required devices, including a high-oxygen nasal cannula or noninvasive positive pressure ventilator, for patients exhibiting any of the risk factors. Maitre et al. [38] and Heunks et al. [39] reported that the use of a noninvasive positive pressure ventilator is useful during bronchoscopy in hypoxemic patients. Furthermore, Lucangelo et al. [40] reported that a high-flow nasal interface could be effectively used in patients with mild respiratory dysfunction during bronchoscopy. This can reduce not only patient discomfort but also the burden on the bronchoscopist. However, further prospective studies are needed to validate our findings.
In conclusion, the results of this study suggest that age >60 years, a low FEV1, and a longer duration of sedation (>40 minutes) are risk factors for hypoxia during bronchoscopy under sedation in adult patients. Therefore, patients with these risk factors should be prepared and cautioned about the complication before they undergo the procedure. Further prospective, multicenter studies are necessary to validate these findings and improve the safety of bronchoscopy under sedation.
Notes
Authors’ Contributions
Conceptualization: Kim YS. Methodology: Choi JS, Kim YS. Formal analysis: Choi JS, Kim YS. Data curation: Choi JS, Kim YS. Investigation: Choi JS, Kim YS. Writing - original draft preparation: Choi JS, Kim YS. Writing - review and editing: Choi JS, Lee EH, Lee SH, Leem AY, Chung KS, Kim SY, Jung JY, Kang YA, Park MS, Chang J, Kim YS. Approval of final manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
This study was supported by a faculty research grant from Yonsei University College of Medicine (6-2015-0068).