Factors Associated with Worsening Oxygenation in Patients with Non-severe COVID-19 Pneumonia
Article information
Abstract
Background
This study aimed to determine the parameters for worsening oxygenation in non-severe coronavirus disease 2019 (COVID-19) pneumonia.
Methods
This retrospective cohort study included cases of confirmed COVID-19 pneumonia in a public hospital in South Korea. The worsening oxygenation group was defined as that with SpO2 ≤94% or received oxygen or mechanical ventilation (MV) throughout the clinical course versus the non-worsening oxygenation group that did not experience any respiratory event. Parameters were compared, and the extent of viral pneumonia from an initial chest computed tomography (CT) was calculated using artificial intelligence (AI) and measured visually by a radiologist.
Results
We included 136 patients, with 32 (23.5%) patients in the worsening oxygenation group; of whom, two needed MV and one died. Initial vital signs and duration of symptoms showed no difference between the two groups; however, univariate logistic regression analysis revealed that a variety of parameters on admission were associated with an increased risk of a desaturation event. A subset of patients was studied to eliminate potential bias, that ferritin ≥280 μg/L (p=0.029), lactate dehydrogenase ≥240 U/L (p=0.029), pneumonia volume (p=0.021), and extent (p=0.030) by AI, and visual severity scores (p=0.042) were the predictive parameters for worsening oxygenation in a sex-, age-, and comorbid illness-matched case-control study using propensity score (n=52).
Conclusion
Our study suggests that initial CT evaluated by AI or visual severity scoring as well as serum markers of inflammation on admission are significantly associated with worsening oxygenation in this COVID-19 pneumonia cohort.
Introduction
Coronavirus disease 2019 (COVID-19) has now become a pandemic since the first case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in Wuhan, China1. The symptoms vary widely, from asymptomatic disease to pneumonia, to life-threatening complications and ultimately death. Sometimes it shows rapid progression of respiratory failure soon after the onset of dyspnoea and hypoxemia2. It is important to unravel the risk factors associated with hypoxemia and identify patients who are susceptible to severe or critical illness upon infection.
Older patients and those with pre-existing respiratory or cardiovascular conditions, diabetes, hypertension, and cancer appear to be at the greatest risk for poor outcomes or severe complications1,3–5. Leucocytosis, low lymphocyte count, serum levels of D-dimer, lactate dehydrogenase (LDH), ferritin, cardiac troponin, and higher concentrations of proinflammatory cytokines were reported to be risk factors associated with severe and fatal COVID-19 in hospitalized patients1,6,7. Typical imaging features of COVID-19 were established to help early screening and evaluation of the severity and extent of disease. Computed tomography (CT) involvement scores can assist in evaluation of the severity and extent of the disease8. Previous studies estimating risk factors included mostly people with severe and fatal diseases at presentation, and data are lacking for subclinical or non-severe COVID-19 patients. We explored potential risk factors associated with worsening oxygenation in a retrospective cohort of patients with non-severe COVID-19 pneumonia.
Materials and Methods
1. Study design and participants
This retrospective, single-center study, recruited hospitalized patients from 30 January to 15 April, 2020 in a public teaching hospital that also served as a COVID-19 dedicated hospital in Seoul, South Korea. We reviewed patients with COVID-19 pneumonia who routinely underwent non-contrast CTs at admission according to the hospital protocol. Ethical approval was provided by the institutional ethics review board of our hospital (2020-04-024). The requirement for informed consent was waived because of the retrospective study design. All those who tested positive SARS-CoV-2 in Korea were either hospitalized or monitored in community isolation settings, and discharged after twice consecutive SARS-CoV2 tests converted to negative. The inclusion criteria were patients aged ≥18 years who (1) were positive for nucleic acid detection of SARS-CoV-2, (2) underwent a chest CT within 24 hours of admission, and (3) showed evidence of viral pneumonia in the initial chest CT scan. The presence of ground-glass opacity (GGO) or consolidation in the bilateral peripheral posterior lungs on chest CT scans without any other specified causes or pathogen in a COVID-19 confirmed patient was categorized as CT-documented COVID-19 pneumonia9. The exclusion criteria were (1) patients with symptom onset more than 14 days; (2) normal findings on initial chest CT; and (3) lung abnormalities other than viral pneumonia.
The clinician’s decision dictated treatment. Multidisciplinary teams screened for signs of acute deterioration and the need for intensive care unit (ICU) admission daily using an in-hospital electronic-medical-record monitoring system.
2. Data collection and definitions
Demographic characteristics of the patients, laboratory and radiological data were reviewed. The need for oxygen devices such as nasal oxygen supply, high-flow oxygen therapy, or respiratory support such as invasive mechanical ventilation (MV) were assessed.
For classification of the clinical course with poor oxygenation throughout the hospitalization, we grouped patients into the worsening oxygenation group and the non-worsening group. The worsening oxygenation group was defined as having any of the following criteria for admission or transfer to the ICU: (1) desaturation event with peripheral oxygen saturation of hemoglobin (SpO2) on room air with rest ≤94% in at least two consecutive measurements or (2) respiratory failure requiring high-flow oxygen therapy or MV. The non-worsening group referred to those who never desaturated and did not need supplemental oxygen.
According to the ‘Diagnosis and Treatment Program of Pneumonia of COVID-19,’ severe cases were defined as having any of the following criteria: (1) respiratory rate ≥30 breaths/min; (2) resting blood oxygen saturation ≤93%; or (3) partial pressure of arterial blood oxygen/fraction of inspired oxygen ≤300 mm Hg. Critical patients needed to meet one of the following conditions: (1) respiratory failure requiring MV, (2) shock, or (3) other organ failure requiring ICU monitoring or treatment10. We defined “non-severe COVID-19 patients” as those who did not meet any of the severe or critical criteria on admission.
3. Chest CT acquisition
Chest CTs were performed using a 64-detector row CT scanner (SOMATOM Sensation 64, Siemens Healthcare, Erlangen, Germany) on admission (low-dose [reference mAs, 40] with automatic exposure control; slice thickness, 1.0 mm; and reconstruction interval, 3.0 mm). Axial images were reconstructed with a sharp reconstruction kernel at a 3 mm slice thickness. The CTs were performed with the patient in the supine position at full inspiration without contrast medium. Axial images were reconstructed with a sharp reconstruction kernel at a 3 mm slice thickness.
4. Quantitative CT analysis
CT images of each patient were uploaded in a free software for artificial intelligence (AI)–driven automatic CT analysis of COVID-19 pneumonia (MEDIP v1.2.0.0, MEDICALIP Co. Ltd., Seoul, Korea), released on a website (http://medicalip.com/mobile/shop/covid19.php) on March 18, 2020. The deep learning software automatically generated a volumetric mask of the lung and pneumonia. The CT parameters from the automatic quantitative software were: the total lung volume (cm3), the pneumonia volume (cm3), pneumonia extent, and the mean lung densities of the total lung and the pneumonia.
An experienced thoracic radiologist (Y.K.L), blinded to the clinical data and laboratory indicators, evaluated the visual severity scores of the CT images. The CT severity score is adapted from a method previously used in patients after severe acute respiratory syndrome11. The extent of lung lesions was scored from 0 to 5 in each lobe and summed up (0, normal; 1, 1%–5% involvement; 2, 6%–25% involvement; 3, 26%–50% involvement; 4, 51%–75%; 5, 76%–100% involvement). The CT severity score was defined as the sum of the individual scores in the five lobes, which ranged from 0 to 25 points.
5. Statistical analysis
Continuous variables were represented as mean and standard deviation or median and interquartile ranges (IQR). A one-sample Kolmogorov-Smirnov test was performed to check the normality of all variables. To compare the two groups, the Mann-Whitney U test was used for continuous variables, and the chi-square or Fisher exact test was used for categorical variables. Correlation analysis was performed to identify associations between continuous variables. Univariate logistic regression analysis was performed to identify the clinical variables associated with worsening oxygenation events. Finally, a propensity score matching analysis was performed to minimize the effect of potential confounding factors that could affect the worsening oxygenation of COVID-19 pneumonia patients. The propensity score was estimated using a non-parsimonious logistic regression, with worsening oxygenation event as the dependent variable and all the characteristics as covariates (sex-, age-, and underlying-disease) based on their methodological, statistical, and clinical relevance. The patients with worsening oxygenation were matched 1:1 with the patients without worsening event according to the propensity score using exact matching. To assess bias reduction using the propensity score matching method, absolute standardized differences were calculated, with a value of >20% indicating a meaningful imbalance in the baseline covariate. We selected 26 matched patients from each group to perform a case-control study at a ratio of 1:1, and a univariate logistic regression analysis was also performed with matched data. All statistical analyses were performed using SPSS statistical software version 23.0 (IBM Corp., Armonk, NY, USA) and R software version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria). p-values were based on a two-sided significance level of 0.05.
Results
1. Demographics and clinical courses of enrolled patients
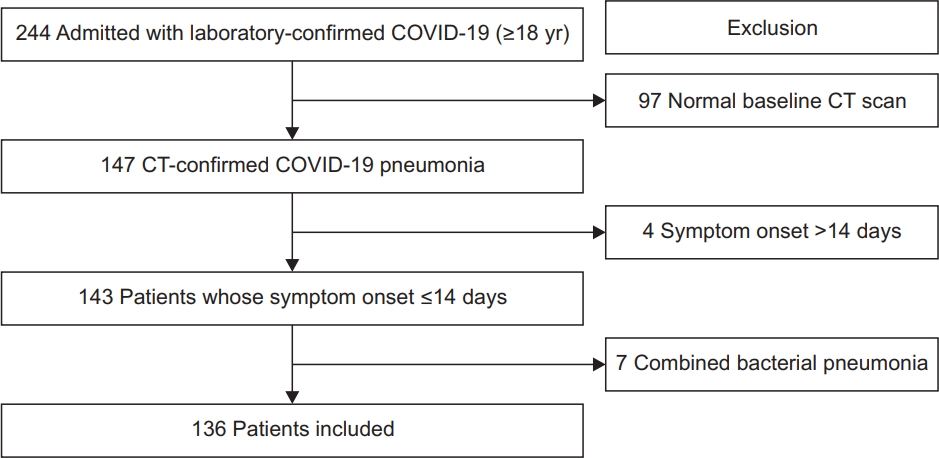
A total of 244 patients were admitted with laboratory-confirmed COVID-19 (Figure 1). After excluding 97 patients with normal baseline CT scans, four patients whose symptom onset was >14 days, and seven patients with bacterial coinfection or mycobacterial disease, 136 patients were included in this study (56 men, 80 women; mean age, 44.8±17.4 years; range, 18–95 years). No patient received MV or high-flow oxygen therapy on admission, only one patient had SpO2 on room air ≤93%, and two patients showed respiratory rate ≥30 breaths/min, there was no shock or organ failure at presentation. Most patients, except for three patients, were classified as having non-severe COVID-19 on admission10.
Among the 136 patients, 32 patients (23.5%) were classified into the worsening oxygenation group, and 104 remained in the non-worsening group (76.5%). All patients in the worsening oxygenation group had oxygen desaturation ≤94% in at least two consecutive measurements, and 10 patients required oxygen supplementation. Only two patients in the worsening oxygenation group needed MV, while a total of five patients needed high-flow oxygen therapy before or without MV. No patient needed extracorporeal membrane oxygenation (ECMO). During hospitalization, 10 patients were admitted to the ICU, including two patients who developed acute respiratory distress syndrome, and one patient died declining to apply the MV in accordance with a previously signed advance directive. Median hospitalized days were 31.4±1.1 without difference among two groups. Among the patients in the worsening oxygenation group, time intervals for oxygen desaturation ≤94% were a median 2 days (IQR, 1–5) from admission and 8 days (IQR, 6–11) from symptom or disease onset, respectively. The oxygen support was started after a median 3 days (IQR, 1–7) from admission and 12 days (IQR 9–13) from symptom or disease onset.
2. Baseline characteristics and laboratory indices between the two groups
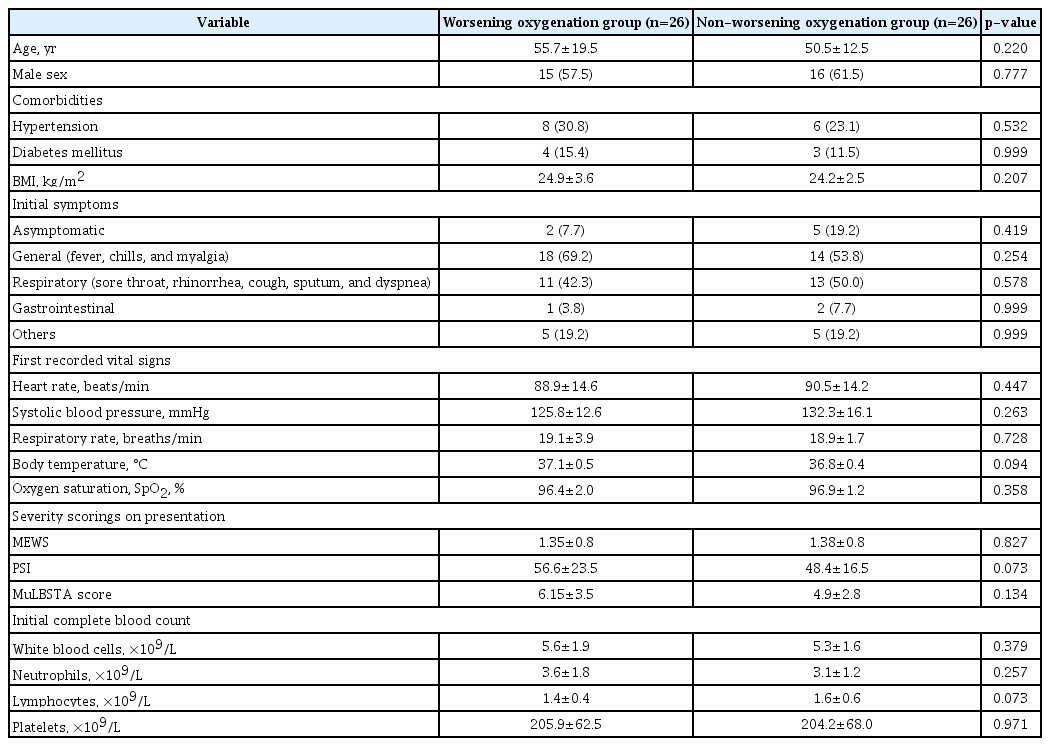
The baseline characteristics of COVID-19 patients according to the clinical course are summarized in Table 1. The average interval for admission from symptom or disease onset was 6.8 days. Only 71 of 136 patients (52.2%) complained of respiratory symptoms, and only 23 of 136 patients (16.9%) had a body temperature (BT) ≥37.5°C on admission. Intervals between symptom or disease onset and admission, and initial symptoms showed no difference between the two groups. The first recorded vital signs were similar in the two groups.
Patients in the worsening oxygenation group were older (p<0.001) and had more underlying diseases than those in the non-worsening group (40.6% vs. 22.1%, p=0.038). Hypertension was the most common underlying disease in both groups, and dementia was more frequent (15.6% vs. 1.0%, p=0.003) in the worsening oxygenation group than in the non-worsening group. The worsening oxygenation group showed higher body mass index (BMI) and 53.1% had obesity based on a BMI ≥25 kg/m2 (vs. 26.9%, p=0.006).
There were numerous differences in laboratory findings between the two groups (Table 1), including higher serum levels of C-reactive protein (CRP), ferritin, and LDH as well as lower lymphocyte counts in the worsening oxygenation group than in the non-worsening group (all p<0.05). The worsening oxygenation group had higher pneumonia severity index (PSI); (56.5 vs. 37.1, p<0.001) and MuLBSTA score (6.0 vs. 3.9, p=0.001) than the non-worsening group, the modified early warning score (MEWS) showed no difference (1.4 vs. 1.3, p=0.737).
3. Relationships between CT features and worsening oxygenation
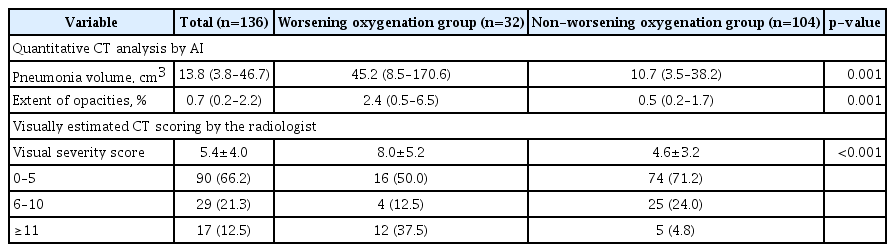
The pneumonia volume quantified using AI was significantly larger in the worsening oxygenation group (median, 45.2 cm3 vs. 10.7 cm3; p=0.001) as well as the extent of opacities (median, 2.4% vs. 0.5%; p=0.001). Visual severity scores of the CT images were also significantly higher in the worsening oxygenation group (8.0±5.2 vs. 4.6±3.2, p<0.001). In particular, 37.5% of the worsening oxygenation group showed a visual severity score ≥11/25 (vs. 4.8% of the non-worsening group) (Table 2).
Figure 2 shows examples of COVID-19 pneumonia lesions from each group detected by free software for AI-driven automatic CT analysis.
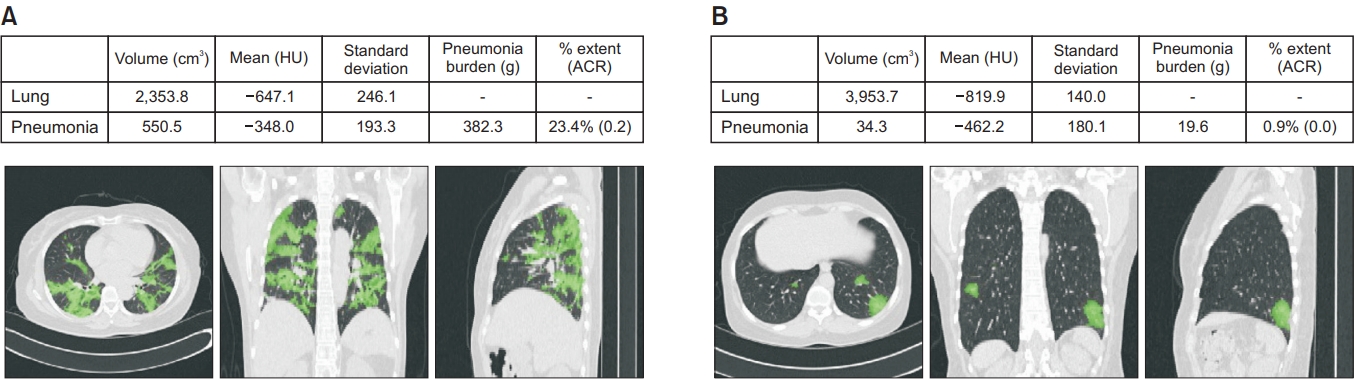
Coronavirus disease 2019 (COVID-19) pneumonia lesions detected by the artificial intelligence (AI) system and comparison of the interpretation of the quantification computed tomography parameters between the worsening oxygenation group (A) and the non-worsening oxygenation group (B). The area considered as COVID-19 pneumonia by AI is highlighted in green. The following images of two patients are illustrated. (A) One is a 55-year-old female who entered the worsening oxygenation group within 24 hours of admission. She presented with desaturation ≤94% within 24 hours of admission and worsened rapidly, requiring high-flow oxygen therapy on the 3rd day after admission. She was discharged on the 42nd day from admission. AI calculated a pneumonia volume of 382.3 g and pneumonia extent of 23.4%. The radiologist scored 19/25 using the visual severity score. (B) The other image shows a 47-year-old female who did not meet the worsening oxygenation group criteria during follow-up and was discharged from the hospital after the 41st day without any respiratory event. AI calculated a pneumonia volume of 19.6 g and pneumonia extent of 0.9%, and the radiologist scored 6/25 using the visual severity score.
4. Predictors of worsening oxygenation
We initially evaluated the results using univariate analysis (Table 3). Our analysis revealed that elderly patients, dementia, obesity, higher pneumonia severity scores, such as the PSI and MuLBSTA score, higher levels of initial CRP, ferritin, and LDH, and lower lymphocyte levels were associated with the worsening oxygenation group compared to the non-worsening group. In addition, pneumonia volume and the extent of the CT by AI, and visual severity scores, were higher in the worsening oxygenation group when compared with the non-worsening group (p<0.05).
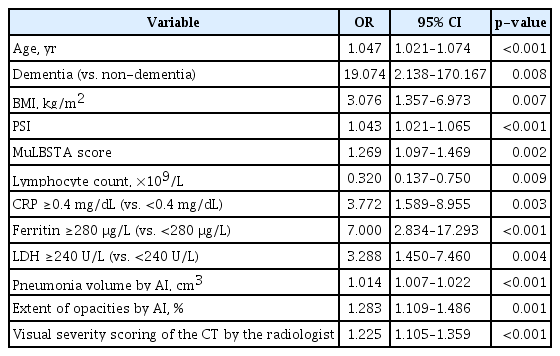
Univariate analysis of predictive parameters for worsening oxygenation in patients with COVID-19 pneumonia (n=136)
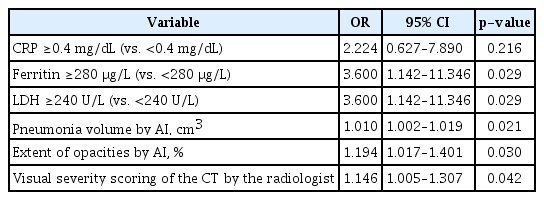
After matching on the propensity score, 52 patients were included in the analysis, and between-group differences for all covariates were eliminated (Table 4). After excluding the impact of age, underlying disease, initial symptoms and first recorded vital signs, initial pneumonia severity scoring, and complete blood count, ferritin ≥280 μg/L (odds ratio [OR], 3.600; 95% confidence interval [CI], 1.142–11.346; p=0.029), LDH ≥240 U/L (OR, 3.600; 95% CI, 1.142–11.346; p=0.029), pneumonia volume (OR, 1.010; 95% CI, 1.002–1.019; p=0.021) and extent (OR, 1.194; 95% CI, 1.017–1.401; p=0.030) by AI, and visual severity scores (OR, 1.146; 95% CI, 1.005–1.307; p=0.042) were the parameters for predicting worsening oxygenation in this cohort (p<0.05) (Table 5).
Discussion
We designed this study to identify parameters at an early stage to predict whether oxygen will decrease. Initial chest CT parameters by AI and visual severity scoring predicted worsening oxygenation in non-severe COVID-19 pneumonia even though initial vital signs at admission were not predictive for worsening oxygenation during hospitalization in our study. It is estimated that 15%–20% of COVID-19 patients develop severe pneumonia and 5%–10% require critical care12. Severe illness of COVID-19 usually begins approximately 1 week after the onset of symptoms2, while patients have variable phases of symptoms and disease onset at admission12. In the present study, most patients were classified as having non-severe COVID-19 at presentation10, and no patient received MV or high-flow oxygen therapy on admission. Patients in this cohort were admitted an average of 6.8 days from symptom onset, and 12.5% were asymptomatic on admission. Nevertheless, 23.5% of these patients proceeded to oxygen desaturation during a median 2 days from hospitalization.
Early case series from the Korean Cohort Study showed that 21.4% of patients received oxygen therapy, with no requirement for MV13. In the Daegu and Gyeongbuk area in Korea, with substantial community outbreaks, a retrospective study (mean age of 55.4±17.1 years) showed that 13.3% of patients required ICU admission with MV use in 11.2%, ECMO in 4.1%, and a mortality rate of 5.1%14. Studies on COVID-19 have been limited to patients with severe or critical disease admitted to the ICU, though a recent report showed that more than 80% of COVID-19 cases were mild in China4,6,15–20. In our study, most cases were non-severe, as evidenced by relatively low rates of ICU admission and mortality rates that would be related to younger ages (mean, 44.8±17.4) and lower comorbidity rates (26.5%) than that of previous reports. In metropolitan Seoul, all confirmed cases were either hospitalized at dedicated hospitals or monitored at community isolation centers. Many cases of COVID-19 were diagnosed by surveillance testing in South Korea, so that a large proportion of the patients in our cohort had non-severe or subclinical symptoms at the beginning of hospitalization.
To our knowledge, markers for the prediction of worsening oxygenation among patients with initially non-severe COVID-19 pneumonia are not defined. In this cohort, only 16.9% showed fever based on a BT ≥37.5°C. Most of the first recorded vital signs were within normal ranges and showed no difference between the two groups, suggesting that the worsening oxygenation cannot be distinguished by initial vital signs. Apart from that, we noted that more patients in the worsening oxygenation group had higher pneumonia severity scores, and several laboratory parameters such as lymphopenia, higher ferritin, and LDH, as well as older age and comorbidities such as dementia and obesity were associated with a worsening oxygenation. Feng et al.10 suggested that the variance of the MuLBSTA score, may have a better predictive value in COVID-19 pneumonia as with this study21. Xie et al.22 suggested that traditional method such as the new early warning score may not help predict patients who will develop respiratory failure in COVID-19. Our data showed no difference in MEWS.
Our results also underline the importance of the integration of CT extent and severity into the management of COVID-19 pneumonia patients. Despite recent advances in molecular viral characterisation, recent evidence does not support a severity or mortality stratification based on viral load dynamics23. However, CT extent or CT features were recognized as important factors for predicting a worsening prognosis23–25. This is consistent with the results of the current study. The rapid development of AI has significantly improved automatic lung segmentation technology, making it possible to quantify the lesions automatically25. Quantitative analysis of CT using AI tools could provide an automatic and objective estimation of the disease burden, facilitating imaging interpretation during the pandemic23. This study aimed to investigate the capability of quantitative CT imaging features combined with traditional clinical biomarkers in predicting progression to worsening oxygenation in the early stages of COVID-19. We used free software and found that the AI-driven parameters of pneumonia volume and extent of the whole lung in the initial chest CT predicted the worsening oxygenation in non-severe COVID-19 pneumonia. Our study suggests the additional benefit of the visual severity scores summing the estimated extent of each lobe and the integration of clinical and laboratory parameters.
This study has limitations. First, it is a single-center retrospective study. In our hospital, the standard cut-off value for admission or transfer to the ICU and change or add-on of antiviral agents was 94% of the SpO2 on ambient air. These criteria should be regarded as empirical, as there is no robust supporting evidence. Second, fewer patients were severe or critical compared to other studies. The majority of the worsening oxygenation group recovered without oxygen or MV, or ECMO. These favorable outcomes may not reflect the full prognosis of patients with COVID-19 in other areas. We did not analyse the factors that could affect outcomes such as regional differences, medical resources, and treatment options we applied as in a clinical trial. In addition, it might be concerned about generalizability as the great majority of the described patients would not be hospitalized elsewhere and are unlikely to undergo CT imaging in routine clinical practice. Nevertheless, these data, including patients with mild symptoms in a relatively early stage, are thought to be useful in predicting parameters for clinical course and triaging patients in real practice. Third, we did not analyze the CT scans at the time of deterioration or follow-up, and the features or patterns with GGO or consolidation. Finally, we did not rule out other causes of the worsening oxygenation such as microthrombi, pulmonary thromboembolism or myocardial injury.
Our study presents initial CT evaluated by AI or visual severity scoring as well as serum markers of inflammation such as ferritin and LDH at admission are significantly associated with worsening oxygenation in non-severe COVID-19 pneumonia cohort.
Notes
Authors’ Contributions
Conceptualization: Kim S, Lee YK. Methodology: Kim S, Hahm CR, Oh DH. Formal analysis: Kim S, Choi H. Data curation: Choi JP, Kang NR. Investigation: Ahn MY, Oh J. Writing-original draft preparation: Hahm CR, Kim S. Writing - review and editing: Kim S, Lee YK, Hahm CR, Oh DH. Approval of final manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
No funding to declare.
Acknowledgments
We thank the members of the Seoul Medical Centre Fight Against COVID-19 Team (SMC-FACT), all members of the department of emergency medicine, and other colleagues in the field. We would like to thank Editage (www.editage.co.kr) for English language editing.