Health-Promoting Behaviors, Health Literacy, and Levels of Knowledge about Smoking-Related Diseases among Smokers and Non-smokers: A Cross-Sectional Study
Article information
Abstract
Background
For generations, cigarette smoking has presented an important public health concern. This study aimed to compare the health-promoting behavior, exercise capacity, physical activity level, health literacy, and knowledge level of smoking-related diseases between smokers and non-smokers.
Methods
The study included 71 smokers (mean age, 32.69±8.55 years) and 72 non-smokers (mean age, 31.88±9.94 years) between the ages of 20 and 60 years. Assessments included a 6-minute walking test (6MWT), Godin Leisure-Time Physical Activity Questionnaire, Health-Promoting Lifestyle Profile II (HPLP-II), Cardiovascular Risk Factors Knowledge Level Scale (CARRF-KL), Asthma/COPD Awareness Questionnaire, the World Health Organization Quality of Life-Bref questionnaire (WHOQoL-Bref [TR]), and Health Literacy Questionnaire (HLQ).
Results
The results from the study show that the number of coronary artery disease risk factors measured significantly higher among the smoker group members when compared to that of the non-smoker group members (p=0.001). Smokers had significantly lower %6MWT distance than non-smokers (84.83±4.72 and 93.45±7.16, respectively; p<0.05). However, there were no significant differences between the smokers and non-smokers in terms of physical activity, CARRF-KL, HLQ, WHOQoL-Bref, and HPLP-II subscales or total scores (p>0.05). Additionally, while only forty-one smokers (57.7%) were active, 48 of the non-smoker group was active (66.7%).
Conclusion
Smokers suffer greater negative effects to their exercise capacity in comparison to non-smokers. Although smokers and non-smokers have similar levels of health literacy and similar levels of knowledge about cardiovascular disease risk factors and obstructive lung diseases, health professionals could continue to further increase individuals’ awareness of smoking-related risk factors and continue to emphasize the importance of physical activity and exercise for protecting cardiopulmonary health.
Introduction
Most of the World Health Organization (WHO) reports on addictive and non-addictive substances state that cigarette consumption and cigarette addiction are a major threat to public health and that more focus should be given on this subject1. The physiological, hemodynamic, and pathological effects of cigarette consumption affect all organs and systems, leading to various systemic and inter-system problems. In particular, smoking has adverse effects on pulmonary and cardiac health due to the toxic and harmful substances in cigarettes. Cigarette consumption is considered one of the main risk factors of many chronic diseases, especially cancer, cardiovascular diseases (CVD) and some like diseases like chronic obstructive pulmonary disease (COPD), lung cancer, asthma, pneumonia, tuberculosis, and pulmonary hypertension2.
Cigarette exposure adversely affects quality of life in many disease groups. It has been shown that active smokers have negative symptomatic health perceptions and decreased quality of life even without active airway limitation or changes in the lungs compared to non-smokers3. Cigarette consumption is also reported to decrease exercise capacity by damaging the vascular endothelial tissue4.
Field observations and cohort studies have revealed a close relationship between smoking cessation skills and health literacy5,6. Low levels of health literacy are one of the reasons for the smoking cessation rate in people of lower socioeconomic status5. Yang et al.7 found that active smokers have less awareness and acknowledgment of the health risks of smoking than non-smokers and former smokers.
International health associations and national health authorities agree that smoking is the most universal and common health problem. In recent years, the Global Alliance Against Chronic Respiratory Diseases has emphasized the importance of chronic respiratory diseases among the world’s most critical health problems, and this approach is supported by Turkish governmental policies8. Since 2006, various initiatives aimed at reducing smoking have been implemented in Turkey, such as prohibiting the sale of cigarettes to minors, smoking in public places, and advertisements and broadcasting programs that promote cigarette smoking9.
Although the health, economic, and social aspects and adverse effects of cigarette consumption and addiction have been revealed in numerous studies, there is ongoing interest among scientists and especially social science researchers regarding why smokers persist in this behavior. In an effort to understand this phenomenon, many questionnaires have been developed and dozens of non-interventional field studies, focus group interviews, and face-to-face in-depth interviews have been conducted. There are few published studies evaluating differences between smokers and non-smokers in terms of exercise capacity, physical activity level, access to health-related information, and their interpretation and application of this information. Therefore, in the present study, we aimed to compare health-promoting behaviors, exercise capacity, physical activity level, health literacy, level of knowledge about smoking-related diseases, and quality of life in smokers and non-smokers. Determining the cardiovascular and pulmonary disease awareness, health-promoting behaviors, and health literacy of smokers may guide health policy-making and public health perspectives on coping with cigarette consumption. We hypothesized that there would be significant differences in these variables between smokers and non-smokers.
Materials and Methods
1. Participants
This cross-sectional study was conducted between June 2019 and November 2019 in the Cardiopulmonary Rehabilitation Unit of the Hacettepe University Faculty of Physical Therapy and Rehabilitation in Ankara, Turkey. Sample size was calculated based on a previous study by Ergin et al.10 Based on the total physical activity scores of smokers and non-smokers in that study, it was determined that at least 63 participants should be included in each group for our study to have 80% strength using the G*Power analysis system (G*Power, ver. 3.1, Heinrich Heine University Düsseldorf, Düsseldorf, Germany) Accounting for potential loss of up to 10%, the recruitment goal was at least 69 people in each group. This sample size calculation was performed11. Seventy-one smokers between the ages of 18 and 65 years and 72 non-smokers similar in age and sex distribution were included in the study. Inclusion criteria for smokers were consuming at least one cigarette every day for the last year, in accordance with the WHO and International Classification of Diseases (ICD) cigarette addiction criteria. The inclusion criteria for non-smokers were having never smoked in their life or never smoked in the last year under the WHO and ICD cigarette addiction criteria12. Other inclusion criteria that applied to all participants were being between 18 and 65 years of age, volunteering to participate in the research, being able to walk and cooperate, and being literate. Individuals having orthopedic, neurological, and neuromuscular diseases that could prevent walking and which may affect the tests and those with any chronic lung disease, any acute cardiovascular events, chronic heart failure, or cognitive impairment were excluded from the study.
Ethical approval was obtained from Hacettepe University Non-Interventional Clinical Research Ethics Committee for the study (approval date: 24 April 2019, approval number: GO 19/445). Participants in the study were informed about the study verbally and written informed consent form was signed.
2. Assessments
The participants’ demographic characteristics were recorded. Cigarette exposure was recorded as pack-years. Among the risk factors of CVD, advanced age (>45 years for men, >55 years for women), hypertension, diabetes, family history of coronary artery disease (CAD), smoking history, physical inactivity, hyperlipidemia, and personality type were recorded. The number of CAD risk factors was calculated13. Body mass index was classified. Waist and hip circumference measurements were made with a standard tape measure. For abdominal obesity and increased risk of CAD, waist circumference cut-off values in our country were reported as >90 cm for women and >100 cm for men. Waist/hip circumference ratio was calculated14.
1) Exercise capacity
Exercise capacity was evaluated using the six-minute walk test (6MWT), which is a submaximal field test. The test is applied in a 30-meter enclosed corridor. Due to the learning effect, it was repeated twice with a half-hour rest interval between the two tests. Before and after the test, the participant’s systolic blood pressure and diastolic blood pressure measured with a manual sphygmomanometer (Erka aneroid clinic 48, Bad Tölz, Germany) and heart rate (HR) and oxygen saturation (SpO2) values measured with a portable pulse oximeter (Jumper, Guangdong, China) were recorded. Perceived dyspnea, leg fatigue, and general fatigue were also assessed using the Modified Borg Scale before and after the 6MWT. The best 6MWT distance was recorded in meters and the percentage of expected 6MWT distance was calculated (%6MWD)15.
2) Physical activity level
The Turkish version of the Godin Leisure-Time Physical Activity Questionnaire was used to assess the participants’ physical activity levels. This questionnaire includes questions about physical activity performed for at least 15 minutes during leisure time and determines how many times strenuous, moderate, and mild physical activity was done in the last week. The total score is calculated using the following formula: total score=(9×strenuous activity)+(5×moderate activity)+(3×mild activity). Total scores ≥24 are classified as active; scores of 14–23 are classified as moderately active, and those ≤13 are classified as insufficiently active/sedentary16.
3) Knowledge of CVD risk factors
The participants’ level of knowledge regarding CVD risk factors was evaluated using the Turkish version of the Cardiovascular Disease Risk Factors Knowledge Level Scale (CARRFKL). The scale consists of 28 questions in total: 4 about the features of CVD, 15 about risk factors, and 9 about the result of a change in risk behavior. Incorrect responses receive no points and each correct response receives 1 point, for a maximum possible score of 28. Higher score indicates a higher knowledge level17.
4) COPD and asthma awareness level
The Asthma/COPD Awareness Questionnaire from the Turkish Ministry of Health Chronic Airway Disorders Prevention Control Program was used for assessment of awareness level about COPD and asthma. Items in the questionnaire are answered with “yes”, “no”, or “not sure” and the results are interpreted by comparing the response percentages to the literature. This questionnaire was used in an extensive field study on COPD and asthma in Turkey18.
5) Health-promoting lifestyle behaviors
Health-promoting behaviors were evaluated using the Turkish version of the Health-Promoting Lifestyle Profile II (HPLP-II)19. The scale measures health-promoting behaviors related to the individual’s lifestyle. The scale consists of 52 items in six subdimensions (spiritual development, health responsibility, physical activity, nutrition, interpersonal relationships, and stress management). Items are scored on a 4-point Likert-type scale: never (1), sometimes (2), often (3), and regularly (4). The total score ranges between 52 and 208, with higher total scores indicating a more health-promoting lifestyle19.
6) Quality of life
The Turkish version of the WHO Quality of Life-Bref questionnaire (WHOQoL-Bref [TR]) comprises four subdimensions: physical well-being, mental well-being, social relationships, and environmental factors. The scale does not have a total score. Scores between 20 and 100 can be obtained for each subdimensions, and the researcher can choose which scores to use. After the raw scores are calculated, percent scores are obtained. The Turkish version has 27 questions (Item 27 is a national question) and when using this scale, the environmental area score is referred to as environment-tr. Higher scores reflect better quality of life20.
7) Health literacy
The Turkish version of the Health Literacy Questionnaire (HLQ) was used to assess the health literacy of the smokers and non-smokers in our study. The HLQ consists of 25 questions in four subdimensions. The total score ranges from 25 to 125. Participants respond to the items using a 5-point Likert-type scale: I have no difficulty (5), I have a little difficulty (4), I have some difficulty (3), I have difficulty (2), and I cannot/am unable (1). Higher scores indicate a higher level of health literacy21.
3. Statistical analysis
Data analysis was done with the SPSS version 18.0 program (SPSS Inc., Chicago, IL, USA). Mean±standard deviation values are given for quantitative variables; percentage and frequency values are given for categorical variables. Comparisons of the smoker and non-smoker groups were analyzed using Student’s t-test (under parametric conditions), Mann-Whitney U test (under nonparametric conditions) for quantitative variables, and chi-square test for categorical variables. Statistical significance was accepted at p<0.0522.
Results
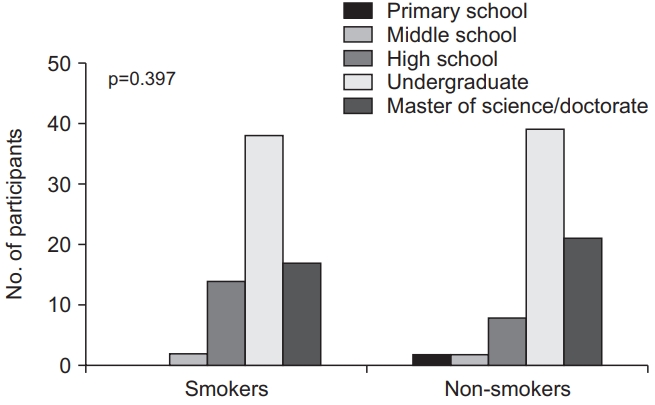
A total of 143 people (71 smokers and 72 non-smokers) were included in the study. Comparisons of the participants’ demographic and clinical data are shown in Table 1. Although the number of CAD risk factors were significantly higher in smokers than non-smokers (p<0.05) (Table 1), seven percentage of smokers (n=5) and 9.7% percentage of non-smokers (n=7) had similar and increased CAD risk according to waist circumference cut-off values (p=0.764). Occupational status differed significantly between the smokers and non-smokers (p=0.005) (Table 1). The marital status was similar between two groups (p>0.05) (Table 1). Educational levels of the smokers and non-smokers are shown in Figure 1 (p>0.05). Alcohol consumption was significantly higher among smokers than those of non-smokers (p=0.026) (Table 1).
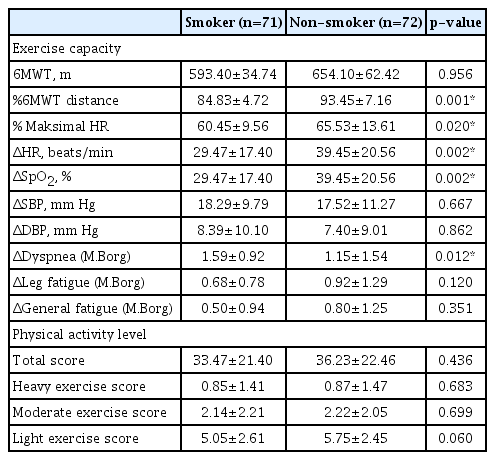
Mean 6MWT distance was similar between the smokers and non-smokers (p>0.05) (Table 2). However, %6MWD and maximum HR during the 6MWT were significantly higher in the non-smokers than the smokers (p<0.05) (Table 2). There were also statistically significant differences between the groups in terms of changes in HR and perceived dyspnea during 6MWT (p<0.05) (Table 2). According to the Godin Leisure-Time Physical Activity Questionnaire, there was no statistically significant difference in physical activity levels between the groups (p>0.05) (Table 2). Forty-one of the smokers (57.7%) were active, 21 (29.6%) were moderately active, and nine (12.7%) were insufficiently active/sedentary, while this distribution in the non-smoker group was 48 (66.7%), 19 (26.4%), and five (6.9%), respectively according to total physical activity score (p=0.409).
The groups’ scores on the CARRF-KL scale and Asthma/COPD Awareness Questionnaire are shown in Supplementary Table S1. There was no statistically significant difference in CARRF-KL scores between smokers and non-smokers (p>0.05) (Supplementary Table S1), while there were some significant differences in terms of asthma/COPD awareness.
The participants’ HPLP-II scores, HLQ scores, quality of life, general health status, and physical, psychological, social, or environmental aspects are shown in Supplementary Table S2.
Discussion
This study shows that although smokers and non-smokers had similar health literacy, health-promoting behaviors, knowledge about CVDs, and physical activity levels, smokers had reduced exercise capacity. Smokers have increased number of CAD risk factors compared to non-smokers. Otherwise, both smokers and non-smokers have a lower overall awareness in some informations regarding chronic respiratory diseases (COPD and asthma) compared to non-smokers.
Despite the development of numerous strategies, the cigarette epidemic has not been conquered yet23. Although some progress has been made in recent years, 26% of the total population and 29% of youth between the ages of 15 and 24 in European Union countries continue to smoke24. A study on people aged 25 and over in Norway demonstrated that people of low socioeconomic status were more likely to smoke and drink alcohol and less able to allocate sufficient time to physical activity25. The prevalence of tobacco consumption was shown to be higher among men and closely associated with alcohol consumption and stress level26. Consistent with the literature, the majority of smokers in our study were men, and higher alcohol consumption was associated with more cigarette consumption. This is related to the fact that cigarette consumption also increases the sensitivity and orientation towards other addictive substances, especially alcohol27.
In a study including 1,200 office workers, Balci et al.28 showed that non-smokers had higher levels of knowledge about CVD risk factors when compared to smokers. The comparable CVD risk factors knowledge in smokers and nonsmokers in our study may be attributable to the low number of participants having CVD risk factors such as hypertension, obesity, and stress, the similar percentage of participants with increased CAD risk, as well as the high education level of study participants (most had undergraduate/postgraduate degrees). Levels of knowledge about asthma and COPD among our study participants were also higher compared to a previous study by Yildiz et al.18. In another study including 230 smokers, nearly half of the participants were not aware of COPD and the young population had the largest proportion of high awareness level29. The high level of knowledge about asthma and COPD in the smokers and non-smokers in our study may be related with the higher education level and younger mean age of our participants. However, there are still some areas for both groups to be informed about lung diseases.
In a 2013 study conducted among teachers, levels of health literacy were lower in those who did not have any chronic diseases and did not use cigarettes and alcohol30. The lower health literacy in smokers was shown to be associated with greater nicotine dependence and lower expectations of adverse outcomes of smoking, independent of demographic characteristics and socioeconomic level5,6. As with COPD/asthma awareness, the comparable health literacy levels in our study groups could be related to the participants’ high education level and younger mean age.
Garrison et al.31 reported that appetizing foods, stress sources, and irritating/disturbing images affect smoking habit and physical activity levels. Boutelle et al.32 showed that smokers engage in less low- and moderate-intensity physical activity. We thought that the main reason for the similar activity levels in smokers and non-smokers was the high numbers of participants who were not employed or held white-collar positions and the younger age distribution in both groups. A study of cardiac patients showed that higher health-promoting behavior scores were associated with male sex, the 49–60 age group, being married, having completed undergraduate or graduate education, higher socioeconomic status, earning an income, and having no additional disease33. To the best of our knowledge, there are no previous studies investigating the relationship between smoking and health-promoting behaviors. The similar HPLP-II scores between smokers and nonsmokers in our study may be because most of the participants were younger, university graduates, married, and were gainfully employed34. Another possible factor is that smokers may have engaged in more health-promoting behaviors in order to protect their health due to their higher CVD risk compared to non-smokers.
Smoking has been shown to reduce exercise capacity in various age groups and sports groups35. Ben Saad et al.36 revealed that individuals using hookahs had a statistically significantly lower 6MWT distance than healthy individuals. Studies in the literature have also revealed that severe lung damage and airway limitation caused by emphysema and chronic bronchitis in smokers increases pulmonary workload37. The lower exercise capacity and increased perceived dyspnea in smokers compared to the non-smokers in our study is compatible with the literature35,36. The decrease in functional capacities affects smokers in many ways, leading to limitations in activities of daily living and loss of work efficiency.
Cheng et al.38 conducted a study of 154 older adults (≥60 years of age) and found that quality of life and exercise capacity were lower among the smokers than non-smokers. It was stated that this age group was more affected by tobacco and tobacco products due to decreased total lung capacities. Demirturk and Kaya39 determined that smokers with regular exercise habits had higher quality of life scores. The lack of difference between the smoker and non-smoker groups may be related to their similar rates of health-promoting behaviors in our study. Even if there was similar quality of life between two groups, the higher overall well-being, physical health, psychological well-being, and total quality of life scores of the nonsmokers were consistent with the literature40.
This study has some limitations. The first limitation of our study was that due to limited resources, we were not able to evaluate the factors limiting the participants’ exercise capacity using a cardiopulmonary exercise test system, which is the gold standard evaluation method. The second limitation of our study was that the proportion of older participants was not large enough to allow generalization of our findings.
In conclusion, exercise performance decreases and dyspnea perception during exercise increases is smoker compared to non-smokers. Physical activity level is preserved in smokers who are mostly young group. Smokers have increased CAD risk and both smokers and non-smokers have a lower knowledge about some informations related with chronic respiratory diseases (COPD and asthma). The data from this study recall the need that any actions and policies to increase levels of health literacy and knowledge of COPD/asthma among both smokers and non-smokers for decreasing their CVD risk and increasing their health-promoting behaviors.
Notes
Authors’ Contributions
Conceptualization: Vardar-Yagli N, Calik-Kutukcu E, Celebi C. Methodology: Vardar-Yagli N, Calik-Kutukcu E, Inal-Ince D. Formal analysis: Calik-Kutukcu E, Bozdemir-Ozel C, Celebi C, Vardar-Yagli N, Saglam M. Data curation: Celebi C, Bozdemir-Ozel C, Calik-Kutukcu E. Writing - original draft preparation: Calik-Kutukcu E, Bozdemir-Ozel C, Celebi C. Writing - review and editing: Saglam M, Vardar-Yagli N, Inal-Ince D, Calik-Kutukcu E, Bozdemir-Ozel C. Approval of final manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
No funding to declare.
Supplementary Material
Supplementary material can be found in the journal homepage (http://www.e-trd.org).
Comparison of knowledge level about cardiovascular disease risk factors, COPD and asthma.
Comparison of health literacy, healthy lifestyle behaviors and quality of life of smokers and non-smokers.