Diagnosis of Pulmonary Tuberculosis and Nontuberculous Mycobacterial Lung Disease in Korea
Article information
Abstract
The recovery of nontuberculous mycobacteria (NTM) from respiratory specimens and the number of patients with NTM lung disease have been rapidly increasing in Korea. An early differential diagnosis of NTM lung disease from pulmonary tuberculosis (TB) is important, as the therapeutic regimen differs from that of pulmonary TB, and it is not necessary to track the contacts of patients with NTM lung disease. However, differentiating NTM lung disease from pulmonary TB remains difficult, because the clinical presentations of the two diseases are similar and a definite diagnosis of NTM lung disease based on sputum culture takes time. This review focuses on the changing epidemiology, clinical and radiographic manifestation, and laboratory diagnosis of pulmonary TB and NTM lung disease in Korea.
Introduction
Nontuberculous mycobacteria (NTM) refer generally to mycobacteria other than Mycobacterium tuberculosis complex (MTB) and Mycobacterium leprae. The prevalence of lung diseases caused by NTM is increasing worldwide, affecting both immunocompetent and immunocompromised individuals1,2. In addition, the distribution of NTM variants is not uniform, and there is marked geographic variability in the prevalence of NTM lung disease and the mycobacterial species responsible3,4.
In Korea, tuberculosis (TB) remains a serious public health problem. In countries with a high TB prevalence, patients whose sputum tests positive for acid-fast bacilli (AFB) on direct microscopic examination or those displaying chest radiographic findings that suggest active TB are generally presumed to have pulmonary TB and are treated empirically with anti-TB drugs. This results in incorrect diagnoses and has led to inappropriate or unnecessary treatment of many patients with NTM lung disease5,6. An early differential diagnosis of NTM lung disease from pulmonary TB is important, as the therapeutic regimen differs from that of pulmonary TB and it is not necessary to track the contacts of patients with NTM lung disease7. However, differentiating NTM lung disease from pulmonary TB remains difficult because clinical presentations of the two diseases are similar and a definite diagnosis of NTM lung disease based on sputum culture takes time7,8.
When NTM are cultured and identified in respiratory specimens, a diagnosis of NTM lung disease requires differentiation from contamination or colonization1,2. Thus, the detection of AFB in respiratory specimens, or the isolation of NTM species, may pose a diagnostic problem for the clinician1,2. In recent years, this issue has become even more relevant, as the frequency of NTM detection in respiratory specimens, as well as the number of patients with NTM lung disease, continues to increase rapidly in Korea.
In this article, we review the changing epidemiology, clinical and radiographic manifestations, and laboratory diagnoses of pulmonary TB and NTM lung disease in Korea.
Changing Epidemiology of Pulmonary TB and NTM Lung Disease in Korea
In Korea, the prevalence of active TB has decreased from 5,065 in 1965 to 1,032/100,000 population in 19959. However, TB is still a major health problem and reported TB cases have not significantly decreased over the last decade10, being 100.6 in 2001 and 87.6/100,000 population in 201211. Unlike TB, NTM lung disease does not have to be reported to public health authorities in most countries, including Korea. Therefore, precise incidence and prevalence data are not available in Korea, although many reports have suggested that the number of patients with NTM lung disease is rapidly increasing in Korea.
The detection of TB cases is based primarily on the microscopic examination of sputum for AFB. This is the simplest and most efficient way to detect sources of transmission. Therefore, patient with AFB-positive sputum is diagnosed to be "bacteriologically confirmed TB case" (previously as "definite TB case")12. However, smear microscopy cannot differentiate between MTB and NTM, which causes a diagnostic dilemma. The recovery rate of NTM from AFB smear-positive sputum specimens is steadily increasing in Korea. In 255 public health centers in Korea, this rate was 6.0% in 2005 and increased to 10.3% in 2011 (Chang-Ki Kim, Korean Institute of Tuberculosis, personal communication). Moreover, this rate is dramatically rising at some referral hospitals in Korea, being 9-12% in 2001-2002 and 45-64% in 2010-201113,14,15.
The proportion of NTM among positive mycobacterial cultures is also increasing in Korea. Before the early 1990s, 97-98% of clinical isolates from sputum specimens contained MTB16. However, after the late 1990s, NTM was isolated from 20-30% of all clinical specimens submitted to mycobacterial laboratory in some referral hospitals16. At some referral hospitals, this rate further increased from about 25-40% in 2001-2002 to about 50-70% in 2010-201114,15,17,18.
The distribution of NTM species varies markedly based on geography3,4. As in other countries, Mycobacterium avium complex is the most common etiologic organism (48-76%) of NTM lung disease in Korea17,18,19. In the past, M. intracellulare was more prevalent than M. avium19,20, but now M. avium is more frequently isolated18,21,22,23. M. abscessus complex (MABC) is the second most common etiologic organism (14-33%) of NTM lung disease in Korea17,18,19,24. Within MABC, M. abscessus (44-53%) and M. massiliense (45-55%) are equally distributed, while M. bolletii is a relatively rare pathogen (1-2%) in Korea25,26,27. In addition, M. kansasii is infrequently isolated and a relatively uncommon cause of NTM lung disease in Korea28,29.
Clinical and Radiographic Manifestations
The classic clinical manifestations of pulmonary TB are chronic cough, sputum production, appetite loss, weight loss, fever, night sweats, and hemoptysis30. However, these non-specific symptoms cannot be used to differentiate between pulmonary TB and NTM lung disease. Moreover, elderly patients with pulmonary TB may have different clinical presentations than younger patients, including more frequent dyspnea and comorbid medical conditions such as cardiovascular disease, diabetes mellitus, and chronic obstructive pulmonary disease31. Previous studies have suggested that some clinical and radiographic characteristics, such as advanced age, history of not smoking, previous TB treatment, absence of pleural effusion, and involvement of middle and/or lower lung zones, are more frequently found in patients with NTM lung disease than those with pulmonary TB7,8. However, there is considerable overlap in the clinical and radiographic features of pulmonary TB and NTM lung disease7,8.
In radiographic manifestations of pulmonary TB in adults, focal or patchy heterogeneous consolidation in the apical and posterior segments of the upper lobes and the superior segments of the lower lobes were most common32. Poorly defined nodules, linear opacities, and cavities are also common findings of pulmonary TB32. In high-resolution computed tomography (HRCT), the most common lesions are centrilobular nodules, tree-in-bud lesions, patchy or lobular consolidations, and cavities32.
NTM lung disease has two different radiographic manifestations: fibrocavitary and nodular bronchiectatic forms1. Fibrocavitary forms of NTM lung disease have cavitary lesions that mostly involve the upper lobes and are similar radiographic features of pulmonary TB1. This type of disease usually develops in older males with underlying lung disease, such as previous TB (Figure 1).
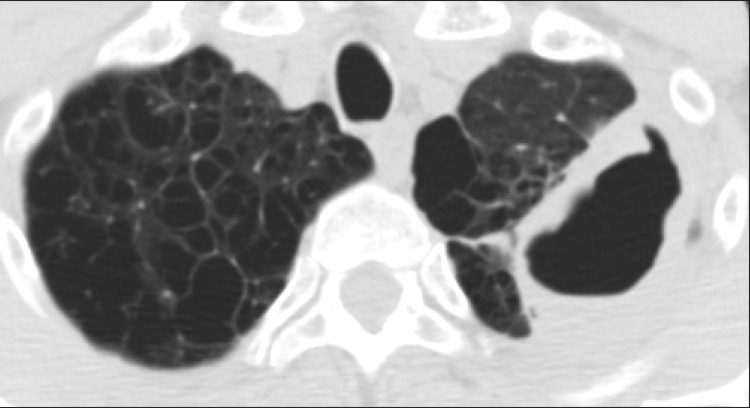
Fibrocavitary form of nontuberculous mycobacterial lung disease in a 53-year-old male with Mycobacterium avium lung disease. Chest high-resolution computed tomography shows a large cavity in the left upper lobe. Note the severe emphysema in both lungs.
Alternatively, NTM lung disease can present with nodular infiltrates that frequently involve the right middle lobe or lingular segment of the left upper lobe (Figure 2). This form of disease is termed nodular bronchiectatic disease, and it occurs predominantly in postmenopausal, non-smoking females and tends to have a much slower progression than cavitary disease1. The nodular bronchiectatic form of NTM lung disease has unique body morphotypes including lower body mass index and body fat, increased height, and increased incidence of scoliosis and pectus excavatum than control subjects33,34. Similar clinical manifestations have also been found in Korean patients35. Although bilateral bronchiectasis and bronchiolitis at HRCT also suggested NTM lung disease, there is considerable overlap in the radiographic manifestations of pulmonary TB and NTM lung disease, and radiographic findings alone could not differentiate the two diseases36.
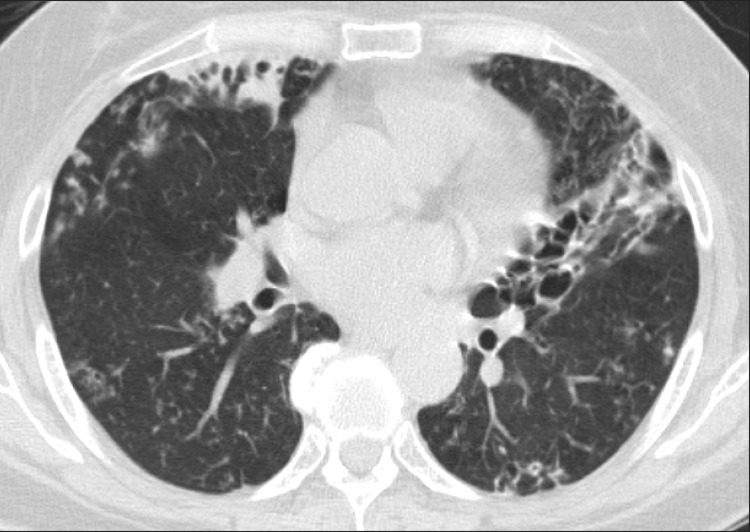
Nodular bronchiectatic form of nontuberculous mycobacterial lung disease in a 60-year-old female with Mycobacterium abscessus lung disease. Chest high-resolution computed tomography shows severe bronchiectasis in the right middle lobe and the lingular segment of the left upper lobe. Note the multiple small nodules suggesting bronchiolitis in both lungs.
To make a diagnosis of NTM lung disease, symptomatic patients with compatible radiographic and HRCT findings should also meet the microbiologic criteria set forth by the American Thoracic Society (ATS)/Infectious Diseases Society of America (IDSA): 1) two positive sputum culture results, or 2) one positive bronchial wash or lavage culture result, or 3) a transbronchial or other lung biopsy yielding positive culture for NTM or compatible histopathological features, such as granulomatous inflammation or stainable AFB, and one positive sputum or bronchial wash culture for NTM1.
Laboratory Diagnosis
In general, AFB staining and culture techniques adopted for MTB are satisfactory for NTM. Smear microscopy cannot differentiate between MTB and NTM. The introduction of nucleic acid amplification (NAA) tests for the detection of MTB directly from clinical specimens has greatly improved TB diagnostics. Currently, many commercial assays use different molecular approaches to amplify and detect MTB. Such tests can confirm the diagnosis of TB more reliably and with higher sensitivity than smear microscopy. Moreover, their high positive predictive values allow discrimination between MTB and NTM in smear positive specimens. If the AFB smear result is positive and the NAA result is negative, the patient can be presumed to have NTM lung disease37. Therefore, NAA tests could be used as an additional test for patients with AFB smear-positive sputum for the rapid detection of MTB and differentiation from NTM.
Ultimately, the diagnosis of NTM lung disease is based on isolation of the organism from respiratory specimens, using solid and liquid media1. The introduction of liquid culture methods has allowed for sensitive detection of both MTB and NTM38. The increased recovery rate is more prominent for NTM than MTB, especially in AFB smear-negative respiratory specimens, when liquid culture methods are combined with solid medium for mycobacterial culture39.
Rapid and accurate identification of MTB and differentiation from NTM in positive culture isolates is essential, particularly because liquid culture is associated with isolation of more NTM39. Commercial MPT64-based immunochromatographic tests and NAA tests are used for this purpose in clinical laboratories in Korea40,41.
Correct identification of species is very important because NTM species differ in their clinical relevance. The methods of identification of mycobacteria in clinical laboratories have changed dramatically over the past two decades. Molecular methods have now surpassed biochemical tests and high-performance liquid chromatography as the method of choice for identifying NTM42,43. Among molecular methods, polymerase chain reaction and restriction fragment length polymorphism analysis using the rpoB gene has been developed for use in clinical practice in Korea44,45. For precise identification of MABC at the subspecies level, as well as uncommonly encountered species, sequencing of some genes including hsp65, rpoB, and the 16S-23S rRNA internal transcribed spacer region is needed46,47,48,49,50,51.
Conclusion
The recovery rate of NTM from respiratory specimens and the number of patients with NTM lung disease has been rapidly increasing in Korea. An early differential diagnosis of NTM lung disease from pulmonary TB is important, as the therapeutic regimen differs from that of pulmonary TB and it is not necessary to track the contacts of patients with NTM lung disease. However, it is not always easy to distinguish NTM lung disease from pulmonary TB, because the clinical and radiographic presentations of the two diseases are similar. As symptoms, radiographic findings, and direct microscopy of respiratory specimens are insufficient to differentiate between pulmonary TB and NTM lung disease, mycobacterial culture and correct identification remain the gold standard.
Acknowledgements
This study was supported by Samsung Biomedical Research Institute grant [SMO1131811].
Notes
No potential conflict of interest relevant to this article was reported.