 |
 |
| Tuberc Respir Dis > Volume 82(3); 2019 > Article |
|
Abstract
Background
Methods
Results
Acknowledgments
Notes
Authors' Contributions:
Conceptualization: Hong SB.
Methodology: Kim WY, Park S.
Formal analysis: Kim HJ.
Data curation: Baek MS.
Investigation: Park S, Baek MS, Chung CR, Park SH, Kang BJ, Oh JY, Cho WH, Sim YS, Cho YJ, Park S, Kim JH.
Writing - original draft preparation: Kim WY.
Writing - review and editing: Park S, Chung CR, Park SH, Kang BJ, Oh JY, Cho WH, Sim YS, Cho YJ, Park S, Kim JH, Hong SB.
Approval of final manuscript: all authors.
Supplementary Material
Supplementary Table S1
References
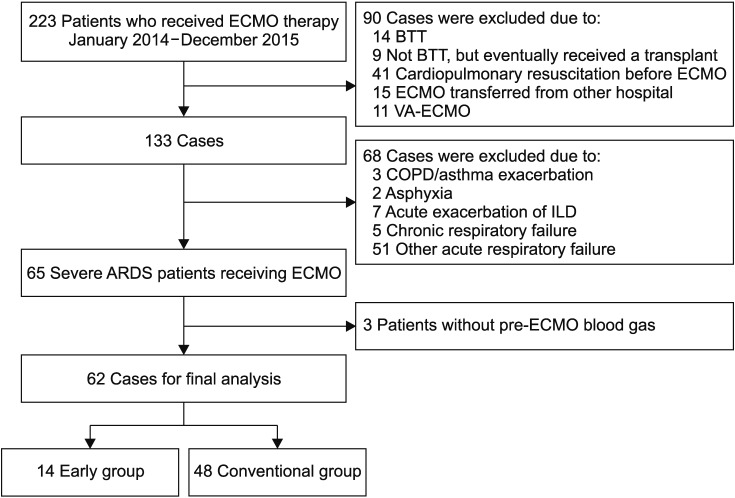
Figure┬Ā1
Illustration of a study flow diagram. ECMO: extracorporeal membrane oxygenation; BTT: bridge to transplant; VA: venoarterial; COPD: chronic obstructive pulmonary disease; ILD: interstitial lung disease; ARDS: acute respiratory distress syndrome.
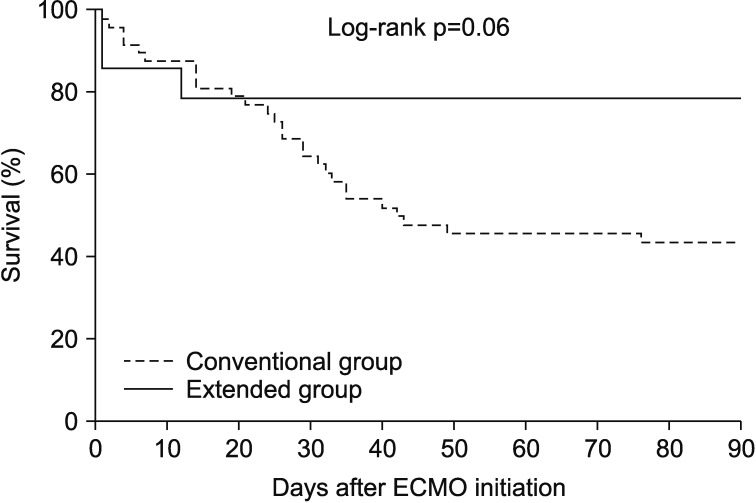
Figure┬Ā2
Kaplan-Meier survival curves of the patients under study. ECMO: extracorporeal membrane oxygenation.
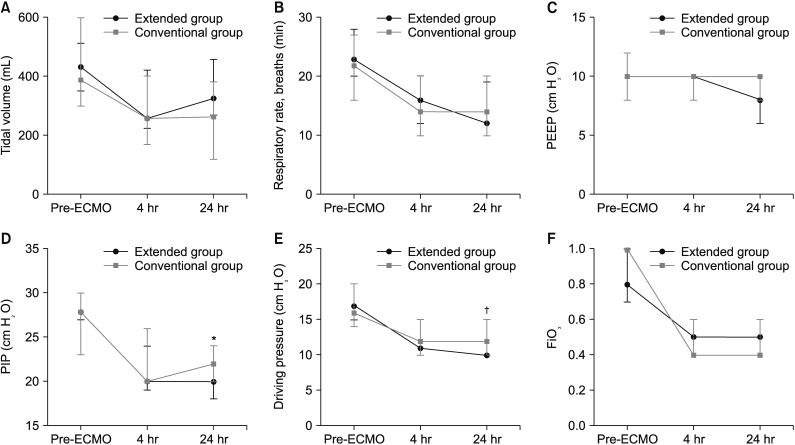
Figure┬Ā3
Serial changes in tidal volume (A), respiratory rate (B), positive end-expiratory pressure (PEEP) (C), peak inspiratory pressure (PIP) (D), dynamic driving pressure (E), and fraction of inspired oxygen (FiO2) (F) in the extended group (dark line) and the conventional group (gray line) during the 24-hour study period. Data is presented as a median value (interquartile range). *p<0.05. ŌĆĀp=0.13. ECMO: extracorporeal membrane oxygenation.
Table┬Ā1
Baseline characteristics of the study patients
Values are presented as median (interquartile range) or number (%).
ARDS: acute respiratory distress syndrome; APACHE: Acute Physiology and Chronic Health Evaluation; ICU: intensive care unit; SOFA: Sequential Organ Failure Assessment; ECMO: extracorporeal membrane oxygenation; MV: mechanical ventilation; PRESERVE: PRedicting dEath for SEvere ARDS on VV-ECMO; RESP: Respiratory ECMO Survival Prediction; FiO2: fraction of inspired oxygen; PaCO2: arterial carbon dioxide tension; PaO2: arterial oxygen tension.
Table┬Ā2
Clinical outcomes of the study patients
Table┬Ā3
Univariate and multivariate analysis of factors associated with 60-day mortality
*Variables with p-values of <0.20 in the univariate analysis were included in the multivariate analysis by using stepwise backward selection procedures.
OR: odds ratio; CI: confidence interval; APACHE: Acute Physiology and Chronic Health Evaluation; ICU: intensive care unit; ECMO: extracorporeal membrane oxygenation; PaO2: arterial oxygen tension; FiO2: fraction of inspired oxygen.
Table┬Ā4
Cox proportional hazards regression model with 60-day mortality as outcome
*Variables with p-values of <0.20 were included in the multivariate analysis using stepwise backward selection procedures.
HR: hazard ratio; CI: confidence interval; APACHE: Acute Physiology and Chronic Health Evaluation; ICU: intensive care unit; ECMO: extracorporeal membrane oxygenation; PaO2: arterial oxygen tension; FiO2: fraction of inspired oxygen.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Supplement
Supplement Print
Print Download Citation
Download Citation




