 |
 |
| Tuberc Respir Dis > Volume 75(5); 2013 > Article |
|
Abstract
Superior vena cava syndrome (SVCS) is usually caused by extrinsic compression or invasion of the superior vena cava (SVC) by malignant tumors involving mediastinal structures. Although thymomas are well-known causes of SVCS, cases of SVCS caused by malignant thymomas protruding into adjacent vessels draining the SVC with thrombosis have been very rarely reported worldwide. We experienced a 39-year-old female patient with SVCS that developed after the direct invasion of the left brachiocephalic vein (LBCV) and SVC by an anterior mediastinal mass with a high maximum standardized uptake value on the chest computed tomography (CT) and positron emission tomography-CT. Based on these results, she underwent en bloc resection of the tumor, including removal of the involved vessels, and was eventually diagnosed as having a type B2 thymoma permeating into the LBCV and SVC. We present this case as a very rare form of SVCS caused by an invasive thymoma.
Superior vena cava syndrome (SVCS) usually occurs either by the extrinsic compression of malignant tumors invading the mediastinum or fibrosing mediastinitis, or by the de novo thrombosis secondary to indwelling central venous devices or some rare occasions of thrombogenic states, such as antiphospholipid syndrome1,2 or Behcet's disease3.
Thymoma is the most common primary tumor arising in the anterior mediastinum and one of the well-known causes of SVCS. The vast majority of SVCS cases caused by thymomas are developed by the extrinsic compression of the superior vena cava (SVC) rather than the direct vascular invasion of the tumor. In addition, although invasive thymoma and thymic carcinoma have a tendency to infiltrate adjacent organs, such as the mediastinal pleura, lungs, pericardium, great vessels and heart4, there are very few reports in the medical literature regarding SVCS caused by an invasive thymoma protruding into the left brachiocephalic vein (LBCV) and SVC with thrombus formation5,6.
A 39-year-old female visited the emergency department suffering from facial edema and dyspnea for 1 week. She was previously healthy and had never received any intravascular procedure in the heart or great veins. An initial neck computed tomography (CT) revealed extensive thrombosis in the LBCV and SVC extending into the right atrium. To define the cause of thrombogenic states, laboratory tests including antinuclear antibody, anticardiolipin antibody, lupus coagulant, protein C and protein S activities, antithrombin III, factor V Leiden mutation, human leukocyte antigen-B51 and skin pathergy test were performed, but all results were normal. Despite anticoagulation treatment with 60 mg of enoxaparin twice a day for 10 days, the extent of SVC thrombosis was not reduced.
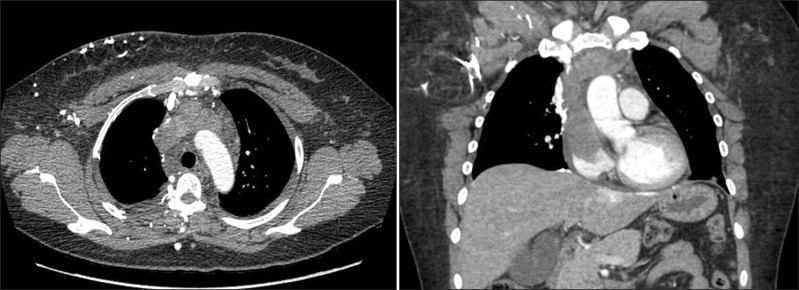
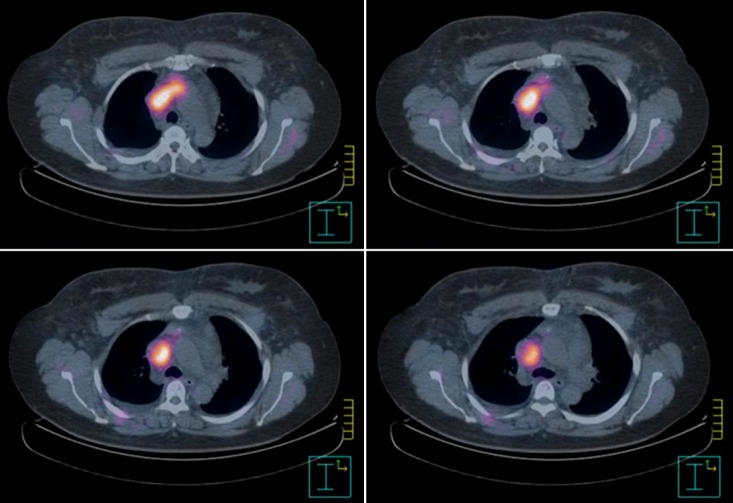
To investigate her underlying pathologic condition, a chest CT was additionally performed, and the anterior mediastinal mass invading the LBCV and SVC was defined (Figure 1). An additional positron emission tomography (PET)-CT performed to evaluate the extent of the mass and the degree of malignancy showed a well-defined hypermetabolic lesion with the maximum standardized uptake value (SUVmax) 6.0 along the LBCV extending into the proximal SVC (Figure 2).
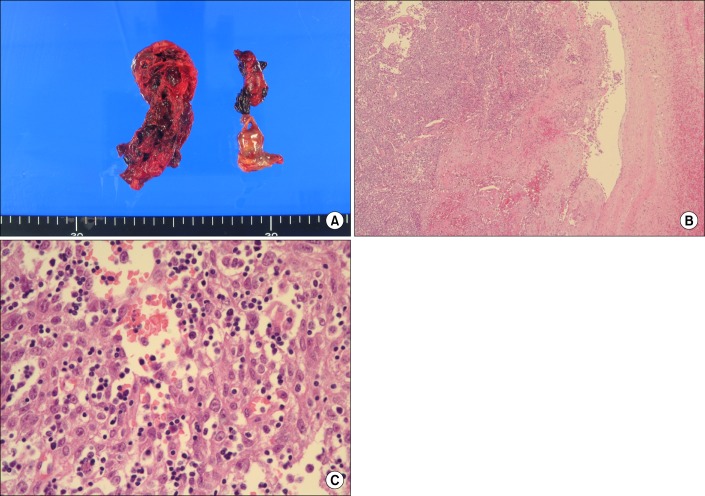
Based on these results, she was presumed to have a malignant mediastinal tumor such as invasive thymoma or thymic carcinoma invading the adjacent great veins, and en bloc resection of the tumor with the involved vessels was performed. Pathologic findings confirmed her diagnosis as a SVC thrombus with type B2 thymoma, a predominantly lymphocytic thymoma with scattered plump cells and vesicular nuclei, invading the LBCV and SVC (Figure 3), and the postoperative stage was defined as III based on Masaoka's classification7.
The patient was discharged from the hospital 16 days after the operation, and has been on the course of postoperative radiation and chemotherapy as adjuvant treatment.
SVCS is the clinical manifestation of various degrees of SVC obstruction and stenosis, with severe reduction in venous return from the head, neck, and upper extremities. About 60% to 90% of SVCS cases have been reported to be caused by the extrinsic compression or invasion of the SVC by malignant tumors, such as non-Hodgkin's lymphoma and small cell lung cancer2, and the de novo thrombosis developed by long-term indwelling intravascular devices and hypercoagulable states are also considered as an important etiology. Our patient was initially diagnosed with SVCS caused by the SVC thrombosis based on her clinical manifestation and the radiologic evidence of the thrombotic occlusion of the SVC. However, the etiology of thrombosis was not clear because of the limited evaluation of the neck CT and normal results of the laboratory tests for thrombophilia. Further tests for the mediastinal mass were needed, and malignant thymomas were suspected prior to the operation based on the results of the chest CT and PET-CT scan.
Thymoma has been known as the most common primary tumor occurring in the anterior mediastinum, but the incidence is estimated to be only 0.15 cases per 100,000 person years in the United States8. Because of the slowly progressing and indolent characteristics of thymomas, patients with thymomas are often asymptomatic9, and, if present, most symptoms result from the mass effect or the invasion of the tumor on adjacent structures10. Although invasive thymoma and thymic carcinoma have a tendency to infiltrate adjacent organs in the mediastinum, almost all SVCS cases by thymomas result from the extrinsic compression by the tumor. By far, SVCS caused by the intravascular permeation with thrombus formation of malignant thymomas have been very rarely reported worldwide4,5,11, and the present case is the first report of SVCS caused by this unusual pattern of invasion in a patient with invasive thymoma in South Korea. The mechanism of this rare form of SVCS was not fully understood, but the thymic veins draining the LBCV have been suggested as possible entrance routes according to previous reports4,5.
With an increasing use of the PET-CT scan, the utility of PET-CT scan in the perioperative evaluation of thymic tumors has been reported in several studies. These studies tried to differentiate the grade of malignancy of thymic tumors using the SUVmax of the tumor or the tumor/mediastinum (T/M) SUVmax ratio defined as the ratio of the peak SUVmax of the tumor to the mean SUVmax of the mediastinum. In these studies, thymomas were classified into low risk (type A, AB, and B1) and high risk (type B2, B3, and C) thymomas based on the World Health Organization (WHO) histological classification12. The results suggested that the SUVmax of 3.5 or the T/M SUVmax ratio of 2.75 were the cut-off value for the differentiation of low risk and high risk thymomas13,14. In this case, the patient was presumed to have high risk thymomas prior to the surgery based on the high SUVmax of 6.0, and the pathologic diagnosis was also confirmed with a high risk (type B2) thymoma as expected.
The treatment of thymomas involves a combination of the surgery, radiation and chemotherapy, but the mainstay of treatment, even for extensive cases, is the surgical resection15. The choice of the combination modality is determined based on the stage of the disease. In cases of stage III and IV diseases7, the standard primary treatment is the surgical en bloc resection with the radiation therapy as adjuvant treatment, and the chemotherapy can be considered as a possible option in the induction and adjuvant settings15. Thymic tumor invasion of the SVC has been regarded as a major determinant of poor prognosis and thus, complete surgical resection including the involved veins is crucial in a successful treatment11. The present case was confirmed with an invasive thymoma with stage III based on Masaoka's classification, which defines macroscopic invasion surrounding the lung, pericardium, SVC, or aorta7. The patient underwent the complete en bloc resection of invasive thymoma with the involved vessels, and the postoperative radiation and chemotherapy has been done as an adjuvant treatment.
In summary, we present a very rare form of SVCS caused by the direct intravascular invasion and thrombus formation of an invasive thymoma. The complete en bloc resection of the tumor is the most important protocol for the successful treatment of the disease, and the postoperative radiation therapy with chemotherapy is expected to improve survival after the operation. The PET-CT scan was valuable in differentiating the grade of malignancy in thymomas and making an adequate surgical plan in perioperative evaluation.
References
1. Herscovici R, Szyper-Kravitz M, Altman A, Eshet Y, Nevo M, Agmon-Levin N, et al. Superior vena cava syndrome: changing etiology in the third millennium. Lupus 2012;21:93-96. PMID: 21844116.


2. Wan JF, Bezjak A. Superior vena cava syndrome. Emerg Med Clin North Am 2009;27:243-255. PMID: 19447309.


3. Yu M, Shi A, Jin B, Jiang X, Liang H, Ouyang C. Superior vena cava occlusion caused by Behcet disease. J Vasc Surg 2012;55:1488-1491. PMID: 22169663.


4. Airan B, Sharma R, Iyer KS, Kalia PK, Singh MK, Shrivastava S, et al. Malignant thymoma presenting as intracardiac tumor and superior vena caval obstruction. Ann Thorac Surg 1990;50:989-991. PMID: 2241393.


5. Terada Y, Ono N, Noguchi T, Kamakari K, Kitano M. A case of thymoma protruding into the superior vena cava through the thymic vein. Ann Thorac Surg 2004;77:1088-1090. PMID: 14992940.


6. Yamazaki K, Takeo S, Takeshita M, Sugimachi K. Thymic carcinoma presenting as an intraluminal growth into the great vessels and the cardiac cavity. Ann Thorac Cardiovasc Surg 2002;8:163-166. PMID: 12472400.

7. Masaoka A, Monden Y, Nakahara K, Tanioka T. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-2492. PMID: 7296496.


8. Engels EA, Pfeiffer RM. Malignant thymoma in the United States: demographic patterns in incidence and associations with subsequent malignancies. Int J Cancer 2003;105:546-551. PMID: 12712448.


9. Schmidt-Wolf IG, Rockstroh JK, Schuller H, Hirner A, Grohe C, Muller-Hermelink HK, et al. Malignant thymoma: current status of classification and multimodality treatment. Ann Hematol 2003;82:69-76. PMID: 12601482.



10. Lewis JE, Wick MR, Scheithauer BW, Bernatz PE, Taylor WF. Thymoma: a clinicopathologic review. Cancer 1987;60:2727-2743. PMID: 3677008.


11. Tseng YL, Wang ST, Wu MH, Lin MY, Lai WW, Cheng FF. Thymic carcinoma: involvement of great vessels indicates poor prognosis. Ann Thorac Surg 2003;76:1041-1045. PMID: 14529981.


12. Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC. Pathology and genetics of tmours of the lung, pleura, thymus and heart. Lyon: IARC Press; 2004.
13. Eguchi T, Yoshida K, Hamanaka K, Shiina T, Koizumi T, Kawakami S, et al. Utility of 18F-fluorodeoxyglucose positron emission tomography for distinguishing between the histological types of early stage thymic epithelial tumours. Eur J Cardiothorac Surg 2012;41:1059-1062. PMID: 22219437.



14. Terzi A, Bertolaccini L, Rizzardi G, Luzzi L, Bianchi A, Campione A, et al. Usefulness of 18-F FDG PET/CT in the pre-treatment evaluation of thymic epithelial neoplasms. Lung Cancer 2011;74:239-243. PMID: 21439670.


15. Davenport E, Malthaner RA. The role of surgery in the management of thymoma: a systematic review. Ann Thorac Surg 2008;86:673-684. PMID: 18640366.


Figure┬Ā1
A massive thrombosis in the left brachiocephalic vein and the superior vena cava extending into the right atrium is observed in the chest computed tomography.
Figure┬Ā2
The positron emission tomography-computed tomography shows hypermetabolic activity with a maximum standardized uptake value of 6.0 for the anterior mediastinal mass and thrombosis.
Figure┬Ā3
(A) The superior vena cava thrombus. Macroscopically, the thrombus is soft and dark red, similar to fish flesh. (B) Microscopically, the tumor cells grow in a solid pattern within the large vessels (H&E stain, ├Ś40). (C) The tumor shows a type B2 thymoma with a predominance of large and polygonal epithelial cells with round or elongated nuclei. Considerable numbers of non-neoplastic small lymphocytes mixed with the tumor can be observed (H&E stain, ├Ś400).
- TOOLS
-
METRICS

- Related articles
-
A Case of Superior Vena Cava Syndrome Caused by Klebsiella Pneumonia.1994 February;41(1)
A Case of Acute Respiratory Distress Syndrome Caused by Nitric Acid Inhalation.2005 December;59(6)
A Case of Acute Respiratory Distress Syndrome Caused By Zinc Fume Inhalation.2007 April;62(4)


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



