 |
 |
| Tuberc Respir Dis > Volume 74(5); 2013 > Article |
|
Abstract
Malignant fibrous histiocytoma, a type of sarcoma, is a malignant neoplasm with uncertain origin that arises in both the soft tissues and the bone. The occurrence of primary malignant fibrous histiocytoma of the pleura is extremely rare. We report a case of a 65-year-old Korean man who is being diagnosed with primary malignant fibrous histiocytoma of the pleura.
Malignant fibrous histiocytoma (MFH) of the pleura is extremely rare1. The first case was reported in 19822. MFH is a soft tissue sarcoma mainly occuring in the soft tissues, especially in the extremities and trunk. MFH is an aggressive malignancy with high potential of local recurrence and distant metastasis3-5. Surgery is treatment of choice even with recurrence and metastasis6. In this report, we present the case of a 65-year-old Korean man who was diagnosed with primary MFH of the pleura. We present the case and literature review about this unusual MFH.
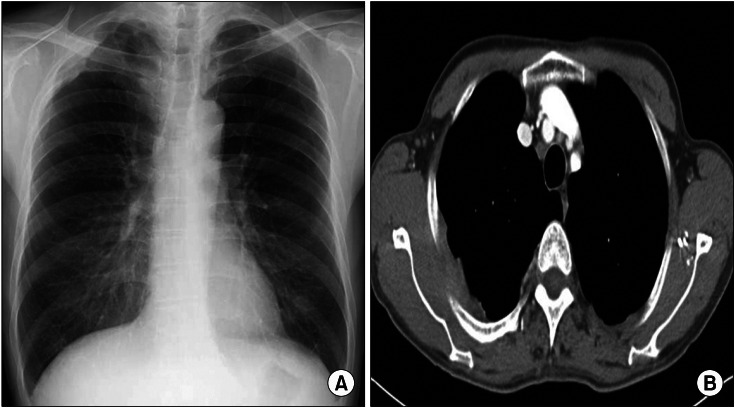
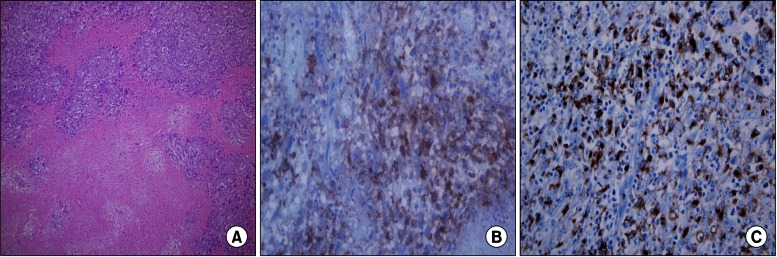
A 63-year-old man presented with dry cough of a 2-week duration. He had a history of pulmonary tuberculosis that had been treated with anti-tuberculosis medication 10 years ago. He was a farmer and former smoker, with 30 pack-years. Physical examination at the time of admission did not indicate any abnormality in the patient. Chest radiograph showed thickening in the right side of the apical pleura (Figure 1A). Chest computed tomography (CT) scans showed diffuse pleural thickening and a mass-like lesion with heterogenous enhancement (Figure 1B). Trans-thoracic needle biopsy was performed to rule out malignancy. Histopathological examination of the biopsy specimen showed anaplastic cytomorphology, with marked nuclear pleomorphism and atypical mitoses. Immunohistochemistry staining was performed. The panel of monoclonal antibodies consisted of CD68, vimentin, calretinin, cytokeratin 5/6 (CK 5/6), CK 7, thyroid transcription factor-1 (TTF-1), CD56, leukocyte common antigen (LCA), CD34, human melanoma black 45, and S-100. The tumor cells were positive for vimentin and CD68 (Figure 2). These cells were immunonegative for all other markers tested, ruling out carcinoma (cytokeratin), sarcomatous mesothelioma (calretinin), solitary fibrous tumor (CD34), and neurogenic sarcoma (S-100 protein).
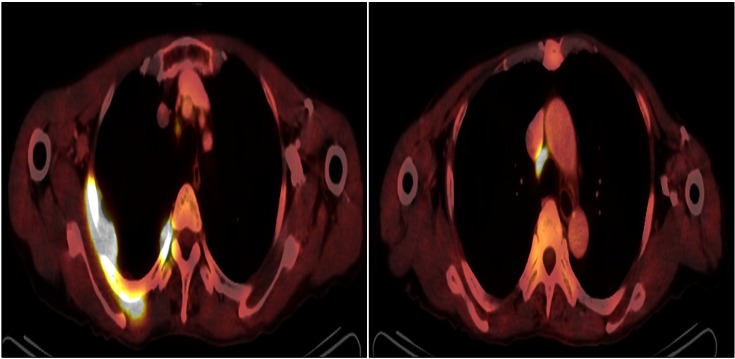
Brain magnetic resonance imaging and bone scan performed for cancer staging showed normal findings. Positron emission tomography-computed tomography PET-CT) showed multinodular hypermetabolic lesion (standardized uptake value, 13.2) at the posterior pleural aspect, with mediastinal lymph node metastasis in the right upper and lower paratracheal nodes (Figure 3). Thus, the final diagnosis was mesenchymal malignancy, primary MFH of the pleura without metastasis beyond the thorax.
The patient underwent thoracotomy with excision of the bulk of the primary mass. The pleural masses on apico-posterior mediastinum which was encountered with third costoverbral joint was resected. Resection of the upper lobe attached to the primary mass, intercostal muscle, right second, third and fourth ribs and mediatinal lymph node dissection was done. The post-operative biopsy result was the same type of the MFH (pleomorphic type) as that of the trans-thoracic needle biopsy performed before the operation. Cancer invasions in lung, ribs, intercostal muscle, vertebra were noted. The patient was discharged after his condition improved but had been lost to follow up since discharge.
MFH is the most common soft-tissue sarcomas in adults. MFH occurs most commonly in the extremities (70-75%), followed by the trunk and retroperitoneum. MFH is characterized by a bimorphic population of fibrocytes and histiocytes usually arranged in a storiform pattern7,8.
Primary pleural MFH is extremely rare9,10. Only one case have been reported in the literature of Korea so far1. There are no typical clinical symptoms, but the patients with pleural MFH usually experience chest pain, cough, and hemoptysis. Their chest radiographs and chest CT usually show diffuse masses of the visceral and parietal pleura. Chest CT is not specific for MFH. There are no suggestive imaging patterns that can be used for the diagnosis prior to biopsy. The exact diagnosis of pleural MFH depends on an accurate differential diagnosis from other malignancy by results of the histopathology and immunohistochemistry. Therefore, the use of an antibody panel is recommended in order to confirm the diagnosis of pleural MFH and to rule out a commonly considered differential diagnosis. Immunohistochemically, MFH are nearly uniformly positive for vimentin, CD68 and negative for calretinin, cytokeratin, TTF-1, CD56, LCA, CD34, and S-100 protein. The identify of CD68 and vimentin, mesenchymal differentiation marker and absence of normal lung tissue in primary mass suggests that MFH is originated in pleura11,12.
MFH has been categorized into five types, based on the histopathologic subtype, including storiform-pleomorphic, myxoid, inflammatory, giant cell, and angiomatoid variants. Since primary pleural MFH is very rarely reported, if it has been diagnosed histopathologically, a comprehensive evaluation should be immediately performed to check whether it is a metastatic tumor originating from the lower extremities and abdomen or a primary tumor. The lung, ribs, intercostal muscle, vertebra were possibility of primary focus because postoperative biopsy result revealed cancer invasions in theses structures. However, the lesion in this case report is primary pleural MFH because imaging modalities, including CT, bone scan, PET-CT revealed no tumors other than the pleural tumor and postoperative pathologic finding suggested cancer invasion of their surrounding soft tissue in addition to bone marrow of rib, vertebra.
Surgery is the cornerstone of treatment for all soft-tissue sarcomas13. The goal of surgery is to eradicate the disease from the affected area. The effect of either chemotherapy or radiotherapy is presently unclear. The prognosis of MFH depend on complete surgical resection with negative microscopic margins, associated to improved disease free specific survival. Prognostic factors that are known to correlate with survival in patients with MFH include tumor grade, depth, size, metastatic status, patient's age, and histologic subtype14. Favorable prognostic factors include age less than 60 years old, tumor size less than 5 cm, superficial location, low grade, the absence of metastatic disease, and a myxoid subtype.
In conclusion, primary pleural MFH is extremely rare tumor and its diagnosis is confirmed by the histopathology and immunohistochemistry. Surgery is treatment of choice of MFH.
References
1. Choi SH, Koh KP, Han JO, Choi JB. Primary malignant fibrous histiocytoma (MFH) of pleura: a case report. Korean J Thorac Cardiovasc Surg 2000;33:770-772.
2. Yang HY, Weaver LL, Foti PR. Primary malignant fibrous histiocytoma of the pleura: a case report. Acta Cytol 1983;27:683-687. PMID: 6316701.

3. Rzyman W, Jaskiewicz K, Murawski M, Sternau A, Marjanski T, Karmolinski A, et al. Primary malignant fibrous histiocytoma of the lung. Thorac Cardiovasc Surg 2007;55:186-189. PMID: 17410507.



4. Kauffman SL, Stout AP. Histiocytic tumors (fibrous xanthoma and histiocytoma) in children. Cancer 1961;14:469-482. PMID: 13751857.


5. Weiss SW, Enzinger FM. Malignant fibrous histiocytoma: an analysis of 200 cases. Cancer 1978;41:2250-2266. PMID: 207408.


6. Belal A, Kandil A, Allam A, Khafaga Y, El-Husseiny G, El-Enbaby A, et al. Malignant fibrous histiocytoma: a retrospective study of 109 cases. Am J Clin Oncol 2002;25:16-22. PMID: 11823689.


7. Russell WO, Cohen J, Enzinger F, Hajdu SI, Heise H, Martin RG, et al. A clinical and pathological staging system for soft tissue sarcomas. Cancer 1977;40:1562-1570. PMID: 907970.


8. Yousem SA, Hochholzer L. Malignant fibrous histiocytoma of the lung. Cancer 1987;60:2532-2541. PMID: 2822221.


9. Maitani F, Fujimori S, Hayashi Y, Hasegawa A, Iwazaki M. A case of juvenile primary pulmonary malignant fibrous histiocytoma. Tokai J Exp Clin Med 2010;35:130-132. PMID: 21319042.

10. Kabiri H, Elfakir Y, Kettani F, Validire P, El Meslout A, Benosman A. Malignant primary fibrous histiocytoma of the pleura. Rev Mal Respir 2001;18:319-322. PMID: 11468596.

11. Cardillo G, Facciolo F, Cavazzana AO, Capece G, Gasparri R, Martelli M. Localized (solitary) fibrous tumors of the pleura: an analysis of 55 patients. Ann Thorac Surg 2000;70:1808-1812. PMID: 11156076.


12. Rais G, Raissouni S, Mouzount H, Aitelhaj M, Khoyaali S, El Omrani F, et al. Primary pleural leiomyosarcoma with rapid progression and fatal outcome: a case report. J Med Case Rep 2012;6:101PMID: 22480303.




13. Williard WC, Collin C, Casper ES, Hajdu SI, Brennan MF. The changing role of amputation for soft tissue sarcoma of the extremity in adults. Surg Gynecol Obstet 1992;175:389-396. PMID: 1440165.

14. Coindre JM, Terrier P, Bui NB, Bonichon F, Collin F, Le Doussal V, et al. Prognostic factors in adult patients with locally controlled soft tissue sarcoma: a study of 546 patients from the French Federation of Cancer Centers Sarcoma Group. J Clin Oncol 1996;14:869-877. PMID: 8622035.


- TOOLS
-
METRICS

- Related articles
-
A Case Report of Primary Mediastinal Malignant Fibrous Histiocytoma1989 December;36(4)
A Case of Primary Malignant Fibrous Histiocytoma of the Lung1987 September;34(3)
A case of primary malignant fibrous histiocytoma of the lung.1991 March;38(1)
A case of primary malignant hemangiopericytoma of the lung.1991 June;38(2)
A case of primary malignant fibrous histiocytoma of the lung.1991 September;38(3)


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



