 |
 |
| Tuberc Respir Dis > Volume 74(4); 2013 > Article |
|
Abstract
We report a 54-year-old woman who presented with a well-defined, homogeneous, and non-enhancing mass in the retrobronchial region of the bronchus intermedius. The patient underwent endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) for histological confirmation. Serous fluid was aspirated by EBUS-TBNA. Cytological examination identified an acellular smear with negative microbiological cultures. The patient was finally diagnosed with bronchogenic cysts by chest computed tomography (CT) and EBUS-TBNA findings. However, 1 week after EBUS-TBNA, the patient developed bronchogenic cyst rupture and pneumonia. Empirical antibiotics were administered, and pneumonia from the bronchogenic cyst rupture had resolved on follow-up chest CT. To our knowledge, this is the first reported case of pneumonia from bronchogenic cyst rupture after EBUS-TBNA.
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is a minimally invasive method for evaluating the intrathoracic lymph nodes and for diagnosing mediastinal lesions accessible via the major airway. This procedure has a high diagnostic value and avoids general anesthesia which is required for mediastinoscopy1. From these, it can be considered that EBUS-TBNA is generally a safe intervention. However, it remains a procedure with possible serious complications.
We here report an uncommon infectious complication of EBUS-TBNA that occurred after puncture of a bronchogenic cyst.
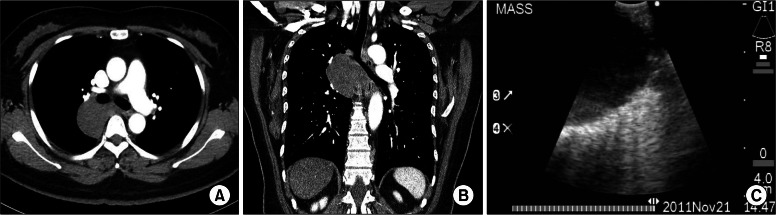
A 54-year-old female patient was referred to our hospital with abnormal chest radiography. She was asymptomatic except for sputum, not purulent, and had a normal physical examination. Contrast-enhanced computed tomography (CT) of the chest revealed a 69-mm-sized, well-defined, homogeneous, and non-enhancing mass in the retrobronchial region of the bronchus intermedius (Figure 1A, B). For further diagnostic evaluation, EBUS was performed using a 7.5-MHz-frequency convex probe bronchoscope (CP-EBUS, BF-UC260F-OL8; Olympus, Tokyo, Japan). A dedicated ultrasound scanner (EU-C2000; Olympus) was used as the image processor. On flexible bronchoscopic examination, there was no endobronchial lesion in the trachea, left or right main bronchus, or bronchus intermedius. On EBUS, an approximately 40-mm-sized low-echogenic mass was seen on the posterior side of the right main bronchus (Figure 1C). Although the ultrasound characteristics were suspicious for a cystic lesion, TBNA was performed for histological confirmation of the mass lesion.
A dedicated 22-gauge needle (NA-201SX-4022; Olympus) was used to puncture and aspirate the lesion under direct visual guidance. Serous fluid was aspirated by EBUS-TBNA. Cytological examination identified an acellular smear with negative microbiological cultures. The patient did not experience any immediate complication such as hemorrhage, pneumothorax, or pneumomediastium from the procedure. The EBUS images correlated with the TBNA aspirate findings, and the patient was diagnosed with bronchogenic cysts.
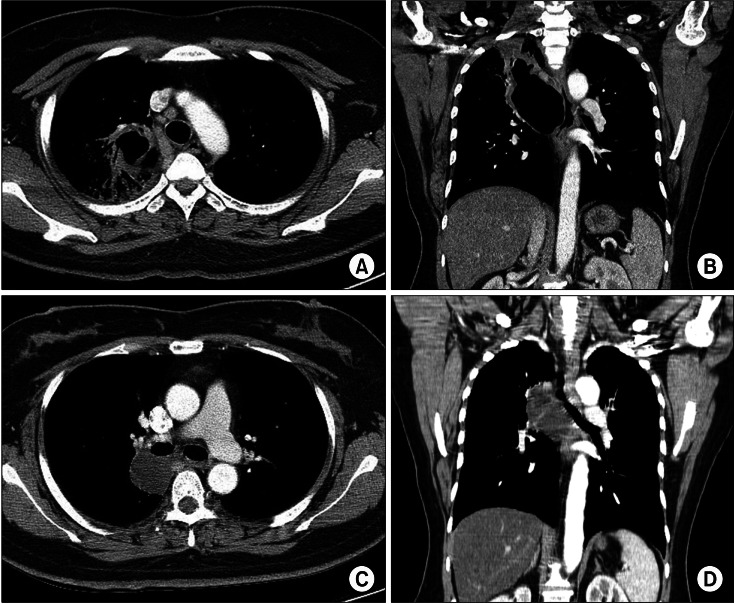
One week after EBUS-TBNA, the patient reported fever, cough, and purulent sputum. A CT scan of the chest revealed a cavitary consolidation communicating with an adjacent bronchogenic cyst that replaced the air space (Figure 2A, B). With a suspected diagnosis of pneumonia from bronchogenic cyst rupture, the patient was started on empirical oral antibiotics. A 3-week course of amoxicillin/clavulanate was prescribed. During the weeks following the event, the size of the consolidation in the right upper lung zone slowly decreased on chest radiography, and the patient was free from symptoms. At 4-month follow-up, chest CT revealed interval improvement of combined pneumonia over the bronchogenic cyst in the right upper lobe (Figure 2C, D). She had no evidence of ongoing infection.
Bronchogenic cysts are lesions of congenital origin derived from the primitive foregut. They are thin-walled, single or multiple, and lined with columnar ciliated epithelium2. The cysts are most commonly located in the mediastinum, and 15-20% occur in the lung. They are frequently present in the lower lobes, are unilocular, are located primarily on the right side, and may contain clear or hemorrhagic fluid, proteinaceous mucus, calcium, or air3,4. Some bronchogenic cysts are asymptomatic and are incidental findings upon radiography; most cysts are symptomatic, and complications are more common in symptomatic patients. Respiratory distress is the most common presentation, manifested by recurring episodes of cough, stridor, and wheezing5-7.
Noninvasive diagnosis of bronchogenic cysts is possible by CT using the typical characteristics of a round, well-circumscribed, usually unilocular mass with smooth outlines2. About half of the cysts are homogeneous, with a near-water density (usually <20 Hounsfield unit [HU] on CT). However, infected cysts that contain proteinaceous material and hemorrhagic cysts can have a more solid appearance (up to 80-90 HU), thereby increasing the diagnostic uncertainty8.
Ultrasound provides excellent delineation between solid and fluid structures. Therefore, EBUS can be used to diagnose bronchogenic cysts that present as soft tissue densities on CT imaging9.
It is recommended that all symptomatic or enlarging cysts be removed surgically. Nevertheless, there is controversy over the appropriate treatment of asymptomatic cysts, given the morbidity and mortality associated with surgical resection. Prophylactic removal of asymptomatic cysts is recommended because a definitive diagnosis can only be obtained by histopathology of resected specimens, and because there are higher rates of complications and the risk for malignant transformation after cysts become symptomatic4,7. Needle aspiration is sometimes considered as a diagnostic method and treatment procedure in patient with bronchogenic cyst. Although this procedure is usually associated with a high recurrence rate because the lining of the cyst is not removed, it remains a possible palliative treatment option in patients presenting with airway obstruction who are poor surgical candidates10. EBUS facilitates visualization during aspiration and enables complete aspiration of the cyst. This causes collapse of the cystic space and may facilitate adhesion between the mucosal surfaces lining the cavity, consequently reducing the recurrence rate10,11.
EBUS-TBNA is a safe and minimally invasive diagnostic technique for evaluating mediastinal lesions1. Complications after EBUS-TBNA in patients with bronchogenic cysts have not been described previously in the English-language literature. To our knowledge, this is the first case report of pneumonia from bronchogenic cyst rupture after EBUS-TBNA. Several recent case studies have demonstrated infective complications after EBUS-TBNA12-15. These infective complications were presumably due to cross-contamination. The working channel of a bronchoscope may become contaminated with airway commensals as it passes through the oropharyngeal region. As a result, when the transbronchial needle passes through the working channel, it also becomes contaminated with microorganisms, which can be directly transferred to the target structures during needle aspiration. Although the needle has an outer sheath to minimize contamination, this sheath still passes through the working channel. These cases indicate that EBUS-TBNA is not free from complications, and bronchoscopists should be aware of potential procedure-related infection.
In conclusion, respiratory physicians performing EBUS-TBNA must be aware that pneumonia can occur after bronchogenic cyst rupture in patients with bronchogenic cyst undergoing EBUS-TBNA.
References
1. Varela-Lema L, Fernandez-Villar A, Ruano-Ravina A. Effectiveness and safety of endobronchial ultrasound-transbronchial needle aspiration: a systematic review. Eur Respir J 2009;33:1156-1164. PMID: 19407050.


2. Takeda S, Miyoshi S, Minami M, Ohta M, Masaoka A, Matsuda H. Clinical spectrum of mediastinal cysts. Chest 2003;124:125-132. PMID: 12853514.


3. St-Georges R, Deslauriers J, Duranceau A, Vaillancourt R, Deschamps C, Beauchamp G, et al. Clinical spectrum of bronchogenic cysts of the mediastinum and lung in the adult. Ann Thorac Surg 1991;52:6-13. PMID: 2069465.


4. Suen HC, Mathisen DJ, Grillo HC, LeBlanc J, McLoud TC, Moncure AC, et al. Surgical management and radiological characteristics of bronchogenic cysts. Ann Thorac Surg 1993;55:476-481. PMID: 8431062.


5. Kanemitsu Y, Nakayama H, Asamura H, Kondo H, Tsuchiya R, Naruke T. Clinical features and management of bronchogenic cysts: report of 17 cases. Surg Today 1999;29:1201-1205. PMID: 10552342.



6. Sarper A, Ayten A, Golbasi I, Demircan A, Isin E. Bronchogenic cyst. Tex Heart Inst J 2003;30:105-108. PMID: 12809250.


7. Aktogu S, Yuncu G, Halilcolar H, Ermete S, Buduneli T. Bronchogenic cysts: clinicopathological presentation and treatment. Eur Respir J 1996;9:2017-2021. PMID: 8902460.


8. McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology 2000;217:441-446. PMID: 11058643.


9. Anantham D, Phua GC, Low SY, Koh MS. Role of endobronchial ultrasound in the diagnosis of bronchogenic cysts. Diagn Ther Endosc 2011;2011:468237PMID: 21747652.




10. Nakajima T, Yasufuku K, Shibuya K, Fujisawa T. Endobronchial ultrasound-guided transbronchial needle aspiration for the treatment of central airway stenosis caused by a mediastinal cyst. Eur J Cardiothorac Surg 2007;32:538-540. PMID: 17629489.



11. Galluccio G, Lucantoni G. Mediastinal bronchogenic cyst's recurrence treated with EBUS-FNA with a long-term follow-up. Eur J Cardiothorac Surg 2006;29:627-629. PMID: 16476541.



12. Haas AR. Infectious complications from full extension endobronchial ultrasound transbronchial needle aspiration. Eur Respir J 2009;33:935-938. PMID: 19336596.


13. Parker KL, Bizekis CS, Zervos MD. Severe mediastinal infection with abscess formation after endobronchial ultrasound-guided transbrochial needle aspiration. Ann Thorac Surg 2010;89:1271-1272. PMID: 20338352.


14. Moffatt-Bruce SD, Ross P Jr. Mediastinal abscess after endobronchial ultrasound with transbronchial needle aspiration: a case report. J Cardiothorac Surg 2010;5:33PMID: 20444284.




15. Huang CT, Chen CY, Ho CC, Yu CJ. A rare constellation of empyema, lung abscess, and mediastinal abscess as a complication of endobronchial ultrasound-guided transbronchial needle aspiration. Eur J Cardiothorac Surg 2011;40:264-265. PMID: 21183356.



Figure┬Ā1
Initial chest computed tomography (CT) and endobronchial ultrasound (EBUS) findings. (A, B) Contrast-enhanced CT before EBUS-guided transbronchial needle aspiration showing a well-defined, homogeneous, and non-enhancing mass in the retrobronchial region of the bronchus intermedius. (C) EBUS image showing a round, low-echogenic mediastinal mass.
Figure┬Ā2
Chest computed tomography (CT) findings after endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA). (A, B) Contrast-enhanced CT at 1 week after EBUS-TBNA showing pneumonic consolidation communicating with an adjacent bronchogenic cyst. (C, D) Contrast-enhanced CT at 4 months after EBUS-TBNA showing interval improvement of combined pneumonia over the bronchogenic cyst in the right upper lobe.


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation




