 |
 |
| Tuberc Respir Dis > Volume 73(4); 2012 > Article |
|
Abstract
Background
We evaluated the clinical outcomes and prognostic factors of patients requiring prolonged mechanical ventilation (PMV), defined as ventilator care for ≥21 days, who were admitted to the medical intensive care unit (ICU) of a university hospital in Korea.
Methods
During the study period, a total of 2,644 patients were admitted to the medical ICU, and 136 patients (5.1%) were enrolled between 2005 and 2010.
Results
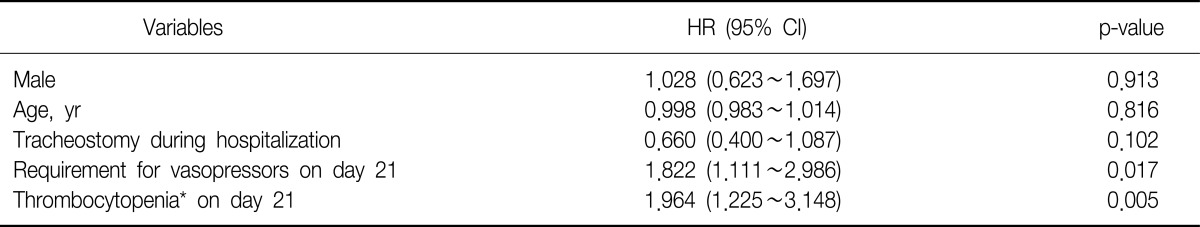
The mean age of the patients was 61.3±14.5 years, and 94 (69.1%) were male. The ICU and six-month cumulative mortality rates were 45.6 and 58.8%, respectively. There were 96 patients with tracheostomy placement after admission and their mean period from admission to the day of tracheostomy was 21.3±8.4 days. Sixty-three patients (46.3%) were successfully weaned from ventilator care. Of the ICU survivors (n=74), 34 patients (45.9%) were transferred to other hospitals (not university hospitals). Two variables (thrombocytopenia [hazard ratio (HR), 1.964; 95% confidence interval (CI), 1.225~3.148; p=0.005] and the requirement for vasopressors [HR, 1.822; 95% CI, 1.111~2.986; p=0.017] on day 21) were found to be independent factors of survival on based on the Cox proportional hazard model.
Advances in critical care have enabled more patients to survive from an acute catastrophic ill state; however these also created a population of patients who were dependent on continuous ventilator care and unable to recover rapidly to a point at which they were fully independent of life support1. The number of patients who require prolonged mechanical ventilation (PMV) has been increasing worldwide, and they were defined as ventilator care for ≥21 days1-10. Several studies reported that these patients consumed a disproportionately high amount of healthcare resources and medical expenses both in the intensive care unit (ICU) and after hospital discharge1-10. There were also several reports regarding prognostic factors for these patients to help physicians determine prognoses by communicating with patients or their surrogates3,11,12.
In Korea, these patients account for a significant portion of the ICU population; there would be distinct clinical characteristics and outcomes because Korea differs from Western countries in many aspects relating to medical expenses, familial support, concept of death, and social customs that would lead to distinctly different characteristics and clinical outcomes. Although there is one previous study that attempted to provide insight on this subset of patients13, it was not representative of our country's population as a whole. Thus little is known about the clinical characteristics and outcomes of patients requiring PMV in our country.
The aim of this study was to investigate the specific patterns of demographic, clinical characteristics and the objective parameter(s) related to poor prognosis in patients requiring PMV in a medical ICU of a university-affiliated tertiary care hospital.
This study was conducted at Pusan National University Hospital, Busan, Korea, a university-affiliated tertiary care hospital with a 12-bed adult medical ICU with full cardiovascular and close airway monitoring, and a separate 7-bed adult coronary care unit. The physician staff in the medical ICU was comprised of 1 full-time specialist, 1 clinical fellow in pulmonary and critical care medicine, 2 resident physicians, and 1 intern. Overnight care was provided by fellow and resident physicians, while the nurse to bed ratio was 1:3. Full-time physical and respiratory rehabilitation therapies were available for all patients. Consultation services were available for all the subspecialists in the hospital.
All data were derived retrospectively from the medical records of patients admitted to the adult (≥18 years old) medical ICU between January 1, 2005 and December 31, 2010. Patients with PMV were defined as those who had undergone mechanical ventilation for longer than 21 days14, regardless of the tracheostomy date. Excluded from the study were patients who had been diagnosed with irreversible brain damage, regardless of length of ICU admission. Two investigators (M.H.K. and K.L.) confirmed that the study objectives and procedures were honestly disclosed and both had full access to all data. The study protocol was approved by the Institutional Review Board (IRB) of the Pusan National University Hospital (E-2011027).
The following data were gathered from the medical records of each patient: age, gender, diagnosis on initial ICU admission, Acute Physiology and Chronic Health Evaluation (APACHE) II scores on day 1 of ICU admission15, length of stay in the ICU and hospital, tracheostomy rate after admission, period from admission to the day of tracheostomy, ventilator weaning rate, ICU and hospital survival, and 6-month survival after ICU admission. The Sequential Organ Failure Assessment (SOFA) score and its components were calculated to quantify the severity of illness based on the degree of organ dysfunction16, and the simplified Therapeutic Intervention Scoring System 28 (TISS) score was calculated to assess the intensity of care on days 1 and 21 of ICU admission17. The Charlson Comorbidity Index was calculated to predict the effect of comorbid disease on patient outcome, acquired from the medical records regarding patient comorbidity before the catastrophic illness requiring ICU care18. All APACHE II, SOFA, TISS scores and Charlson Comorbidity Index were calculated from the raw data collected during chart review by the authors. Survivors were defined as patients who had survived for 6 months after ICU admission. Patients discharged without documentation of a post-discharge follow-up examination were contacted by telephone to determine the length of survival. Successful ventilator weaning was defined as breathing without assistance.
Statistical analyses were performed using the SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Descriptive results were expressed as mean and standard deviation or medians with range. Student's t-test was used to compare the continuous variables and the Chi-square or Fisher's exact tests (for small expected cell sizes) were used to compare categorical characteristics. Patient survival was analyzed using the Kaplan-Meier method, and compared using the log-rank test. The factors found to be significantly associated with survival were analyzed further with a Cox proportional hazard model to adjust for the potential confounding effect of each factor. Hazard ratios with 95% confidence intervals were used to report the results. A two-tailed p<0.05 was considered to indicate a significant difference.
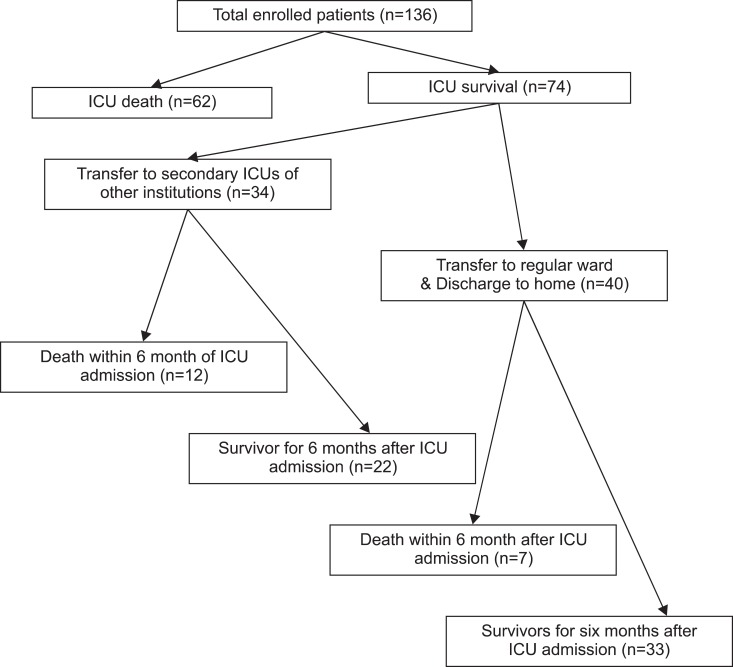
During the study period, a total of 2,644 patients were admitted to the medical ICU. Of those, 136 patients (5.1%) met our definition of PMV patients. The median number of days on mechanical ventilation was 45 (range, 21~231). Clinical characteristics of the patients are shown in Table 1. The most common diagnosis of initial ICU admission was respiratory failure caused by pulmonary causes (n=97) which included pneumonia (n=69), acute exacerbation of chronic lung disease (n=15), pulmonary tuberculosis (n=9), and pulmonary edema (n=4). The medical ICU and hospital mortality rates were 45.6% and 48.5%, respectively, and the 6-month cumulative mortality rate was 58.8%. There were 96 patients who underwent tracheostomy placement after admission and their mean period from admission to the day of tracheostomy was 21.3±8.4 days (median, 22 days; range, 1st day~50th day after admission). Among the 96 patients with trachesotomy after admission, 57 subjects (59.3%) had their placement date after 21 days of mechanical ventilation. Sixty-three patients (46.3%) were successfully weaned from ventilator care; however, we could not find any factors that were associated with successful weaning from ventilator (data not shown). Of the ICU survivors (n=74), 34 patients (45.9%) were transferred to other hospitals (not university hospitals), but there was no significant 6-month cumulative mortality difference compared to patients who were transferred to the general ward (Figure 1).
Aforementioned clinical factors in data collection were evaluated with regard to their influence on survival. Three factors were associated with mortality based on Kaplan-Meier survival curves and log-rank tests (p<0.05): thrombocytopenia (platelet count≤150×109/L) (p<0.001), requirement for vasopressors on day 21 (p=0.007) and tracheostomy during hospitalization (p=0.025). After adjusting for age and sex, these three factors were introduced into the Cox regression hazard model, which revealed that two variables (thrombocytopenia and requirement for vasopressors on day 21) were independent factors of survival (Table 2, Figure 2). Patients (n=57) with at least one of two factors had higher APACHE scores on admission day (25.3±7.2 vs. 22.9±6.6, p=0.044), TISS scores on day 21 (31.2±4.8 vs. 27.9±3.4, p<0.001) and 6-month cumulative mortality rates (75.4% vs.46.8%, p=0.001) than patients without these two factors.
In this analysis of a cohort of patients with PMV, our findings were within the range compared to published studies that demonstrated the incidence of PMV patients and ventilator liberation rates in ICU2-4,6,7,13. Our study also showed a reduced 6-month cumulative mortality rate as compared to previous reports on Korean PMV patients13, which may have been due to the skilled care and advanced various medical resources of critical care. In the future, the number of patients requiring PMV is likely to increase continuously due to new therapeutic strategies and medical resources available in critical care, and would be an emerging challenge for the health care system in Korea. There is a limited amount of data about these patients in our country, thus it would be necessary to evaluate demographic and clinical characteristics through a large prospective study using a formal definition for PMV.
The definition of PMV is defined differently in other studies as ventilator care for ≥4 days with tracheostomy2,6, because the placement of a tracheostomy for patients with prolonged weaning failure is a clinical marker of the transition between the acute and chronic phases of critical illness. From the current study result, however, the period from admission to the day of tracheostomy was not constant. Also, more than half of the total number of subjects received tracheostomy after 21 days of mechanical ventilation which suggested that the day of tracheostomy and its placement may be influenced by differences of opinions between physicians and families of the patients. Therefore, it seems to be appropriate to define patients requiring PMV as those on mechanical ventilation for ≥21 days based on a consensus conference in order to obtain clear and concise clinical characteristics14.
Considering the high symptom burden of these patients and frequent poor outcomes, a mortality prediction model that identifies patients on PMV with the highest and lowest risk for death would be useful to inform discussions of prognoses among clinicians and patients or their family. Recently, a 1-year mortality prediction model was developed for these patients using clinical variables measured on day 21 including thrombocytopenia, requirement for vasopressors, hemodialysis and age ≥50 years3. Of these variables, the former two factors (thrombocytopenia and requirement for vasopressors on day 21) were prognostic indicators in the present study; however the remaining two factors (hemodialysis and age≥50 years) were not. In addition to this model, it was suggested that the long-term prognosis also would be influenced by various factors such as functional or cognitive recovery as well as the opinions of patients' family and physician-family communication6,19-21. There were also cultural differences between Western countries and Korea to be taken into consideration for providing life support; therefore it would be necessary to develop a new mortality prediction model through a multicenter study which would be applicable to the Korean patient population requiring PMV.
This study had several limitations. First, we expected that the concentration of vasopressors and degree of thrombocytopenia would affect outcomes; however, we were unable to identify any statistically significant differences, possibly due to the small sample size. Second, we could not complete interviews for survivors and survey the general conditions (such as quality of life) of the total number of enrolled patients which could have provided more significant results. Third, the study was an observational retrospective analysis and the sample size was small, in that the results of our study may not be generalized. Our data represented the experience of a single center and reflected a unique organization and process of care.
In conclusion, we found that patients requiring PMV had high 6-month cumulative mortality rates and two clinical variables measured on day 21 (thrombocytopenia and requirement for vasopressors) may be associated with prognostic indicators. Prospective, large-scale multicenter studies with longer follow-up time periods are required to determine the distinct demographic and clinical characteristics as well as prognostic factors in the Korean patient population.
Acknowledgements
This work was supported by clinical research grant from Pusan National University Hospital (2011).
References
1. Nelson JE, Cox CE, Hope AA, Carson SS. Chronic critical illness. Am J Respir Crit Care Med 2010;182:446-454. PMID: 20448093.



2. Cox CE, Carson SS, Lindquist JH, Olsen MK, Govert JA, Chelluri L, et al. Differences in one-year health outcomes and resource utilization by definition of prolonged mechanical ventilation: a prospective cohort study. Crit Care 2007;11:R9PMID: 17244364.



3. Carson SS, Garrett J, Hanson LC, Lanier J, Govert J, Brake MC, et al. A prognostic model for one-year mortality in patients requiring prolonged mechanical ventilation. Crit Care Med 2008;36:2061-2069. PMID: 18552692.



4. Lone NI, Walsh TS. Prolonged mechanical ventilation in critically ill patients: epidemiology, outcomes and modelling the potential cost consequences of establishing a regional weaning unit. Crit Care 2011;15:R102PMID: 21439086.



5. Hung MC, Lu HM, Chen L, Hu FC, Chan SY, Yan YH, et al. Life expectancies and incidence rates of patients under prolonged mechanical ventilation: a population-based study during 1998 to 2007 in Taiwan. Crit Care 2011;15:R107PMID: 21457550.



6. Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Ann Intern Med 2010;153:167-175. PMID: 20679561.



7. Wu YK, Tsai YH, Lan CC, Huang CY, Lee CH, Kao KC, et al. Prolonged mechanical ventilation in a respiratory-care setting: a comparison of outcome between tracheostomized and translaryngeal intubated patients. Crit Care 2010;14:R26PMID: 20193057.



8. Robson V, Poynter J, Lawler PG, Baudouin SV. The need for a regional weaning centre, a one-year survey of intensive care weaning delay in the Northern Region of England. Anaesthesia 2003;58:161-165. PMID: 12622105.


9. Zilberberg MD, Luippold RS, Sulsky S, Shorr AF. Prolonged acute mechanical ventilation, hospital resource utilization, and mortality in the United States. Crit Care Med 2008;36:724-730. PMID: 18209667.


10. Cox CE, Carson SS, Govert JA, Chelluri L, Sanders GD. An economic evaluation of prolonged mechanical ventilation. Crit Care Med 2007;35:1918-1927. PMID: 17581479.



11. Dematte D'Amico JE, Donnelly HK, Mutlu GM, Feinglass J, Jovanovic BD, Ndukwu IM. Risk assessment for inpatient survival in the long-term acute care setting after prolonged critical illness. Chest 2003;124:1039-1045. PMID: 12970035.


12. Carson SS, Bach PB, Brzozowski L, Leff A. Outcomes after long-term acute care. An analysis of 133 mechanically ventilated patients. Am J Respir Crit Care Med 1999;159(5 Pt 1):1568-1573. PMID: 10228128.


13. Lee K, Hong SB, Lim CM, Koh Y. Sequential organ failure assessment score and comorbidity: valuable prognostic indicators in chronically critically ill patients. Anaesth Intensive Care 2008;36:528-534. PMID: 18714621.


14. MacIntyre NR, Epstein SK, Carson S, Scheinhorn D, Christopher K, Muldoon S, et al. Management of patients requiring prolonged mechanical ventilation: report of a NAMDRC consensus conference. Chest 2005;128:3937-3954. PMID: 16354866.


15. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818-829. PMID: 3928249.


16. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996;22:707-710. PMID: 8844239.



17. Miranda DR, de Rijk A, Schaufeli W. Simplified Therapeutic Intervention Scoring System: the TISS-28 items: results from a multicenter study. Crit Care Med 1996;24:64-73. PMID: 8565541.


18. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-383. PMID: 3558716.


19. Nelson JE, Mercado AF, Camhi SL, Tandon N, Wallenstein S, August GI, et al. Communication about chronic critical illness. Arch Intern Med 2007;167:2509-2515. PMID: 18071175.



20. Cox CE, Martinu T, Sathy SJ, Clay AS, Chia J, Gray AL, et al. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med 2009;37:2888-2894. PMID: 19770733.



21. Song T, Kim K, Koh Y. Factors determining the establishment of DNR orders in oncologic patients at a university hospital in Korea. Korean J Med 2008;74:403-410.
Figure 2
Survival curves according to the requirement for vasopressor and thrombocytopenia on day 21 for patients requiring prolonged mechanical ventilation. (A) Requirement for vasopressor or not (log rank, 7.26; p=0.007). (B) Thrombocytopenia or not (log rank, 11.27; p=0.008).
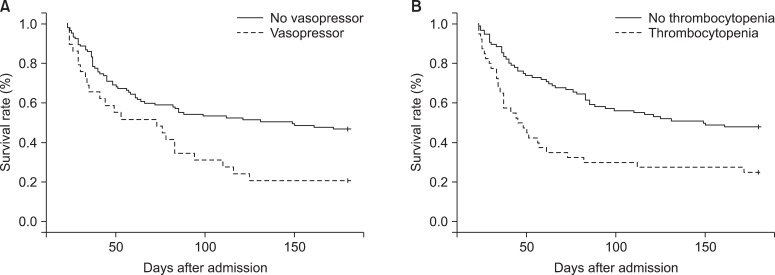
Table 1
Clinical characteristics of enrolled patients
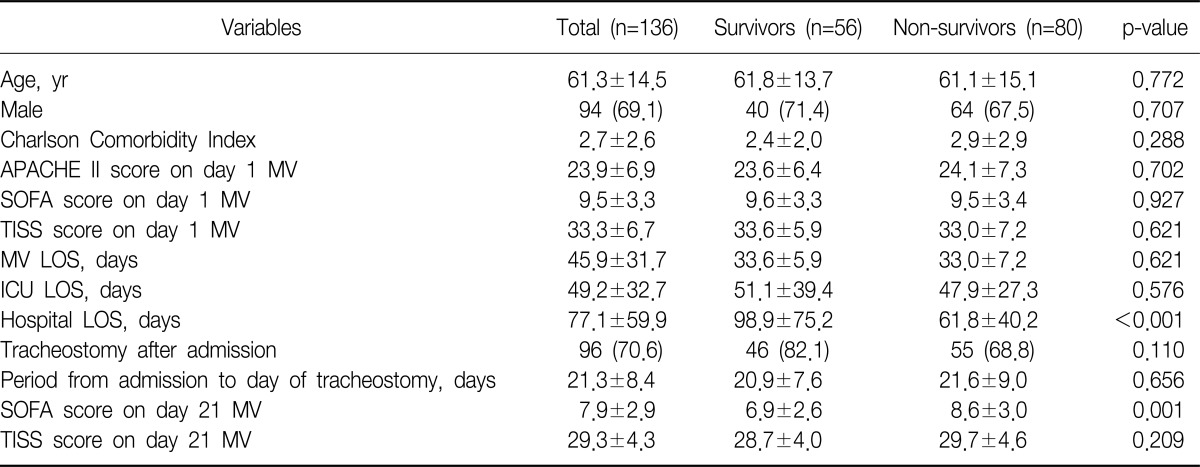
Values are presented as mean±standard deviation for continuous variables and number (%) for categorical variables. Statistical significance was tested by Student's t-test for continuous variables or the Chi-square test or Fisher's exact test (for small numbers) for categorical variables.
APACHE: Acute Physiology and Chronic Health Evaluation; MV: mechanical ventilation; SOFA: Sequential Organ Failure Assessment; TISS: Therapeutic Intervention Scoring System 28; LOS: length of stay; ICU: intensive care unit.


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation




