Perception of Long-Term Oxygen Therapy for Chronic Lung Diseases May Affect Poor Adherence in Korea
Article information
Abstract
Background
Long-term oxygen therapy (LTOT) improves the survival of patients with hypoxemia due to chronic respiratory diseases. The clinical outcomes of LTOT are strongly associated with patient adherence. To improve the adherence of patients, physicians have focused on the efficacy of LTOT. However, poor adherence may stem from patients’ perceptions of LTOT. Herein we evaluated patients’ perceptions of LTOT affecting adherence.
Methods
We conducted a cross-sectional survey study using descriptive, open, and closed-ended questionnaire. Patients using oxygen therapy (OT) or requiring it but avoiding OT responded to the questionnaires at three university hospitals.
Results
Seventy-nine patients responded to the questionnaires. The number of patients using home and portable OT was 69 (93%) and 37 (46.3%), respectively. Patients with good adherence were 22 (30.1%). Among patients with good adherence, 90.9% used oxygen according to physicians’ prescriptions whereas only 37.3% of those with poor adherence followed physicians’ prescriptions (p<0.01). The reasons for avoiding using home OT were fear of permanent use (50%), unwanted attention (40%), and lack of symptoms (40%). They avoided portable OT because of unwanted attention (39%), heaviness (31.7%), and lack of symptoms (21.6%).
Conclusion
Patients on LTOT had the perception of the misunderstanding the effects of OT and of psychosocial barriers to initiate or use LTOT. Considering these findings, health professionals need to provide effective education on the purpose of LTOT to improve patient adherence to OT and provide sufficient support for the management of psychosocial barriers in patients using LTOT.
Introduction
Chronic hypoxemia is a major complication of advanced chronic respiratory diseases, such as chronic obstructive lung disease (COPD), interstitial lung disease (ILD), and lung cancer. Chronic hypoxemia is associated with decreased quality of life, exercise capacity, and increased mortality [1,2]. Long-term oxygen therapy (LTOT) has been recommended by international guidelines for decades at these stages of chronic lung disease [3,4].
Using LTOT for at least 15 hr/day improves survival in patients with chronic resting hypoxemia. Evidence of LTOT based on a randomized controlled trials in the early 1980s, the Medical Research Council (MRC) study, revealed a higher survival rate of 5 years after randomization in severely hypoxemic patients with COPD receiving supplemental oxygen therapy (OT) for >15 hr/day compared to the survival of those without OT [5]. In clinical practice, LTOT is commonly prescribed for other diseases such as ILD, cor pulmonale, cardiac disease, or neuromuscular disease using the same criteria used for COPD [6,7].
National and international guidelines recommend LTOT in the presence of appropriate criteria, which are defined as a resting partial pressure of oxygen in arterial blood (PaO2) of 55 mm Hg or oxygen saturation (SaO2) of 88% or a resting PaO2 between 55 and 60 mm Hg with evidence of pulmonary hypertension, cor pulmonale, or polycythemia with a hematocrit value more than 55%. Patients with a peripheral oxygen saturation (SpO2) below 88% at rest also qualify [3,8].
Patients with good compliance with LTOT tend to have good clinical outcomes, such as requiring fewer hospitalizations [9]. However, a significant number of patients discontinue treatment without reevaluation [10-12]. Factors contributing to persistently poor compliance remain unclear. Despite several reports on the efficacy and compliance to LTOT in patients, most studies have focused on physicians’ views of prescription patterns or medical efficacy [8,9]. Only a few studies have considered the patients’ perspectives, usually using text analysis of structured interviews [13,14]. These studies showed that patients use oxygen as a tool for symptom management; however, the improvement in breathlessness by oxygen does not always meet expectations as perceived by patients. Factors affecting adherence may stem from patients’ perceptions of OT. In this study, we investigated patients’ perceptions of LTOT in a real-world clinical setting in Korea.
Materials and Methods
This cross-sectional survey study used descriptive open and closed-ended questionnaires. The survey was conducted at three university hospitals between December 1, 2017, and April 30, 2018. Patients older than 16 years with chronic hypoxemia due to chronic lung diseases who were currently using OT according to the LTOT criteria or who were required to use oxygen according to the LTOT criteria but avoided it, were included. Patients who did not meet the LTOT criteria and those who received OT after treatment for acute respiratory distress were excluded. The questionnaire was developed by five pulmonary specialists. The questionnaire consisted of 16 items, including five items on the timeframe of oxygen use and prescriptions of oxygen. The questionnaire included a benefit and adverse effects that patients experienced. There were also questions about patients’ perception of avoidance of home oxygen and portable oxygen use. The Korean and English versions of the questionnaire are provided in the Appendices 1, 2.
1. Statistical analysis
All continuous variables were described as standard deviations (SDs), and categorical variables were reported as absolute numbers and percentages. Categorical values were analyzed using the chi-squared test or Fisher’s exact test. In all comparisons, p-values <0.05 were considered statistically significant. All statistical analyses were performed using the SPSS version 25.0 (IBM Corporation, Armonk, NY, USA) for Windows (Microsoft Corporation, Redmond, WA, USA).
2. Ethical statement
This study was approved by the Institutional Review Board of the Inje University Paik Hospital, South Korea (IRB No.17-0177). All participants provided written informed consent before participating in the study. The study was conducted in accordance with the guidelines of the Declaration of Helsinki regarding the rights and dignity of participants.
Results
1. Baseline characteristics of patients with LTOT
Seventy-nine patients responded to the questionnaire on LTOT. Seventy-four patients used home or portable OT, 69 (93.2%) of whom used home OT and 37 (50%) used portable OT, respectively. Among patients using home OT, 32 (46.4%) used both OT (Figure 1). Among the five patients who used only portable OT, three had discontinued home OT and the remaining two patients had never used home OT. Among the five patients who needed to use LTOT but avoided using it, four had never used any OT, and one had previously used home OT. The mean±SD age was 69.8±8.9 years and 53 (67%) were men. The underlying respiratory diseases included COPD (n=41), ILD (n=22), bronchial asthma (n=10), tuberculosis destroyed lung disease (n=6), bronchiectasis (n=4), and others (n=4). Baseline forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC) and FEV1/FVC of patients were 62.4%±21.1%, 45.3%±20.1%, and 57.1%±26.1% of predicted. There were no significant differences between good and poor adherence groups. The details of the variables are shown in Table 1.

Oxygen devices of patients who currently use oxygen therapy. Results are described as numbers. The number of patients using home and portable long-term oxygen therapy (LTOT) was 69 and 37, respectively. five patients who used only portable LTOT, three had discontinued home LTOT and the remaining two patients had never used home LTOT.
2. Benefits and uncomfortable aspects of LTOT according to adherence
Among the 69 patients currently using home OT, only 20 showed good adherence to OT for more than 15 hr/day. Another 49 showed poor adherence to OT for less than 15 hr/day. In the poor adherence group, 28 patients had an OT less than 8 hr/day. Most patients in both the good and poor adherence groups answered that they felt better after using the LTOT. Sixty-nine patients used home oxygen; 59 (85.6%) reported that they experienced benefit of OT. The benefits in the good and poor adherence groups were relief from shortness of breath (85% vs. 83.7%, p=0.521), improvements in quality of life (30% vs. 30.6%, p=0.976), and increased activity after using oxygen (20% vs. 30.6%, p=0.364). The most uncomfortable aspects of using home OT were noise (60% vs. 48.9%, p=0.448), inconvenience of moving (45% vs. 48.9%, p=0.621), and local adverse effect such as of dry mouth (30% vs. 24.5%, p=0.694) (Table 2). In terms of portable OT, 33 (89.2%) considered portable OT was helpful. The uncomfortable aspects of portable OT in the good and poor adherence groups were device-related complication: the associated heaviness (73.3% vs. 70%, p=0.829) and short battery life (80% vs. 45%, p=0.036) (Table 3).
3. How to use LTOT according to adherence
Among patients responded to the questionnaire on LTOT, 73 patients responded their timeframe of the oxygen. Patients with good adherence who used oxygen for more than 15 hr/day were 22 (30.1%). Most patients with good adherence underwent LTOT according to their physician’s prescription (90.9%). Conversely, among 51 (69.9%) with poor adherence who used oxygen for less than 15 hr/day, only 37.3% used OT according to their physicians’ prescription (p<0.01). A total of 34.7% of the patients used OT when they experienced dyspnea without conforming to the physician’s prescription. Patients with poor adherence used OT 17.6% of used OT only during sleep and 9.8% used it when they did daily activities (Figure 2).

How to use long-term oxygen therapy (LTOT) according to adherence. Results are described as number (%). Most patients with good adherence underwent LTOT according to their physician’s prescription (90.9%). Conversely, among patients using oxygen therapy (OT) with poor adherence, only 37.3% used OT according to their physicians’ prescription (p<0.01). *p<0.01. †Good compliance means when patients use OT for more than 15 hr/day. ‡Poor compliance means when patients use OT for less than 15 hr/day.
4. Reason for avoiding oxygen therapy
Patients responded their perceptions on avoiding OT. Among them, patients requiring home OT but avoiding it were 10. Five of them currently used only portable oxygen devices, four had never used any OT and one had used home oxygen devices but used no oxygen devices currently. The reasons for avoidance were fear of permanent use (n=5, 50%), unwanted attention (n=4, 40%), not feeling hypoxemia despite the presence of hypoxemia (n=4, 40%), and cost (n=3, 30%). Patients requiring portable OT but avoiding it were 41 (37 patients currently used only home OT, and four had never used any OT), The reasons for avoiding portable OT were: unwanted attention (n=16, 39%), heaviness during ambulation or moving (n=13, 31.7%), not feeling symptoms despite the presence of hypoxemia (n=8, 21.6%), and the fear of permanent use (n=5, 19.5%) (Figure 3). Perceptions of patients who were reluctant to use home or portable OT were in Supplementary Table S1.
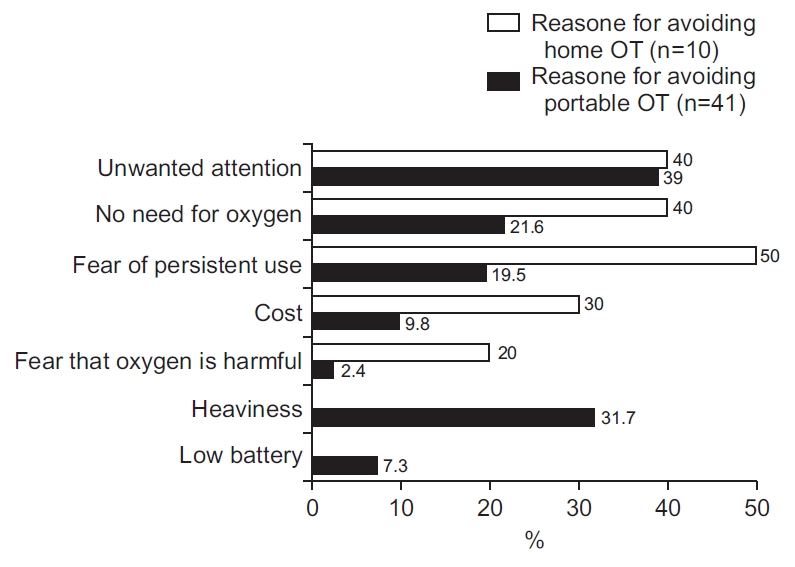
The reasons for avoiding oxygen therapy (OT). Results are described as number (%). Patients who needed to use home OT but avoided it consisted of five patients who currently used only portable oxygen devices, four patients who never used any OT, and one patient who had used home oxygen devices but used no oxygen devices currently. Patients who were reluctant to use portable OT who were consisted of 37 patients who currently used only home oxygen devices and four patients who never used any oxygen devices.
Discussion
As insurance covers LTOT, its use continues to increase [15]. There is an increasing demand for the evaluation of LTOT with respect to intended medical effects as well as medical factors associated with compliance from the physicians’ perspective. To our knowledge, this is the first study to provide patients’ perspectives on LTOT in Korea. This study explored how patients feel and experience the LTOT in their lives.
LTOT improves survival in patients with severe hypoxemia who receive supplemental OT for more than 15 hr/day [4,5]. Ringbaek et al. [9] reported that home OT reduced the hospitalization rate from 92.7% to 63.8%. This benefit was particularly notable in the good compliant group. Previous domestic studies have exhibited good compliance more than 50% of patients who used OT for >15 hr/day and 15.4% who used OT for <8 hr/day [10,15,16]. Our study revealed poor adherence: only 30.1% of patients used OT for >15 hours, and 40.8% used OT for <8 hours. Since the study that reported 52% compliance was conducted before insurance coverage, these patients were considered to need OT because of physicians’ decisions or their own complaints of dyspnea, even though they did not meet the current insurance criteria [10]. Another study that reported improvement compared with those reported by the former study included patients with diseases that did not meet the insurance criteria for OT [16]. Their underlying disease included advanced lung cancer. As a result, 72% of the patients died within 1 year and 92% died within 2 years. All these studies were conducted single-center setting. However, our multicenter study includes patients with chronic lung diseases who used oxygen according to the LTOT criteria. This suggests that compliance with OT may vary depending on the underlying disease and the region. In a recent study, oxygen prescriptions for patients with neuromuscular diseases were more common than oxygen prescriptions for patients with chronic respiratory disease according to National Health Insurance Service data in Korea [17]. The characteristics of OT were considered not only for patients with hypoxemia, but also for those with underlying diseases and their severity.
In previous domestic studies, none or 38% of patients used portable oxygen [15,16]. Conversely, 46.4% of the respondents who used home oxygen also used portable oxygen. This finding may be attributed to the increased insurance coverage. In Korea, the National Health Insurance System extended insurance coverage to portable OT on January 1, 2017. As the economic burden decreased, the use of portable OT increased.
In our study, most patients felt that their symptoms had improved. More than 80% of the patients responded that their shortness of breath improved in both the good and poor adherence groups. The patients in both groups experienced local adverse effects related mouth and nose symptoms. However, no significant differences were observed between the good and poor adherence groups. In a recent domestic study, 36% patients voluntarily discontinued OT [15]. The cause of discontinuation was discomfort with OT, such as a dry mouth or nose. The number and types of local adverse effects were similar to those reported in previous studies, despite large differences in populations concerning underlying respiratory diseases, medical insurance coverage, and equipment types [18-20]. These adverse effects are often neglected or left untreated by physicians [8]. The reason for persistent local adverse effects could be that the majority had not been treated or discussed with healthcare professional [20]. Many commonly reported adverse effects can be treated, which could lead to a potentially positive effect on LTOT.
The most uncomfortable aspects of using portable oxygen were device-related complaints such as battery, noise, weight, and tube length. The longer patient used a portable oxygen device, the more uncomfortable they experienced that the short battery life. The battery was operated for approximately 3 hours depending on the flow at the pulse dose setting, and the recharge time was approximately 3 to 4 hours. The average noise was approximately 25 to 48 dB for home oxygen devices and about 42 to 48 dB for portable oxygen devices. Their average weight was approximately 3 kg, as measured using a portable oxygen device. The oxygen flow rate was approximately 1 to 3 L/min in a portable OT pulse dose setting. The tube lengths were 2.1 and 1.2 m for the home oxygen device and the portable device, respectively. Technical improvements were made to the oxygen devices, but the patients still experienced discomfort. While further development is necessary, inadequate guidance regarding the device may persist discomfort to use LTOT. Tubing length is a predictor of severe physical inactivity and time spent sitting [21]. Aguiar et al. [18] reported that a tubing length of 30 m did not lower the fraction of inspired oxygen supplied and may provide greater freedom for patients to move around at home. Further studies on the appropriate standards for oxygen devices are needed.
In our study, 90% of the patients with good adherence responded that they used oxygen according to the physicians’ prescription. However, among patients with poor compliance, only 36.7% conformed to physicians’ prescriptions. Patients with poor adherence reported that they used oxygen only when they experienced dyspnea (34.7%) or when they slept or engaged in activities of daily living (18.4% and 10.2%, respectively). This finding emphasized that patients with poor adherence misunderstood the medical role of OT. As a medical treatment LTOT improves the survival of patients with severe hypoxemia. Instead of considering OT as a medical treatment and following physicians’ prescriptions, patients with poor adherence used OT as a symptom reliever for complaints of dyspnea. A study on patients’ perceptions of OT conducted in the United Kingdom, reported a common misunderstanding that oxygen was commonly administered to relieve dyspnea [14]. In a previous domestic study, the reason for voluntary cessation of OT was the relief of subjective symptoms [15]. In the same study, the objective parameters of dyspnea did not differ significantly between the enrolled groups, such as the MRC scale and visual analogue scale. Physicians have focused on objective parameters related to compliance 8,9 . However, difference may not lay in objective medical effect but inpatients’ subjective perceptions. Patients’ perceptions of the purpose of OT could be the decisive factor in adherence.
In our study, the most common reason for avoiding home or portable oxygen was unwanted attention from onlookers. No significant differences were observed in terms of good or poor adherence. In one study, participants generally expressed that portable oxygen concentrators were helpful but received unwanted attention [22]. Williams et al. [23] noted that oxygen made their illness visible. Public use of OT seems to threaten the self-image of patients using both home and portable OTs [24,25]. The largest study on the adverse effects associated to LTOT, conducted in 1998, reported that patients using LTOT felt negative self-conscious [19]. Regardless of whether compliance is good or poor, the use of LTOT tends to be associated with a psychological barrier of significant self-consciousness and a sense of social stigma that makes patients feel weak and sick [26]. Consequently, negative self-image may be compromised, leading to embarrassment, worsening social isolation, and decreased patient adherence. Healthcare professionals provide sufficient support for the management of psychosocial barriers in patients using LTOT.
In our study, 50% of patients reported fear of dependency on OT as a reason for avoidance when requiring home OT, compared to 19.5% of patients with portable OT. Fear of dependency on OT was also related to reluctance among patients who had never used OT. One article reported that using oxygen was symbolic of a permanent decline in disease status or worsening of patients [27]. Patients with severe COPD recognize initiation of OT as a key milestone in the disease trajectory and in declining health [28,29]. LTOT is a marker of the terminal lung status and is often synonymous with disability and death. OT can demonstrate the recognition of disease severity, away from the unrealistic expectations about a better prognosis. The initial reaction to OT was fear of recognizing the severity of their disease and death. This psychosocial barrier may be the primary challenge in initiating LTOT in patients with advanced respiratory diseases.
Restriction of ambulation in daily living was another source of discomfort identified in our study. A previous study reported that the most prevalent adverse effects of LTOT are reduced mobility and physical activity [20]. Several studies have reported that OT may be associated with low physical activity in daily life [30,31]. Participants who used the LTOT show less independence in their activities of daily living [21,32]. The ambulation restriction did not appear to restrict the movements imposed by the stationary device. The patients identified their weaknesses and felt trapped in their lungs. Restricted activities of daily living are associated with depression and poor health status [24]. In some cases, depression gets intense and makes the individuals suicidal [33].
This study has several important implications. In clinical practice, to improve the adherence of patients, physicians have focused on objective factors or the medical efficacy of LTOT. However, most patients in both the good and poor adherence groups reported benefits and disadvantages associated OT. Both groups experienced improvement in their symptoms and revealed no evidence of deteriorating compliance with the use of oxygen due to adverse effect. We found that an important difference was patients’ misunderstanding of the effects of OT. However, in a previous study on physicians’ perspectives on home oxygen, physicians mainly emphasized the persistent use of home oxygen for >15 hours or not using too much oxygen [34]. The patients’ perceptions in our study highlight the need for health professionals to manage their perceptions of why they need oxygen. We found the psychosocial barriers that the patients in both good and poor adherence groups. Although it did not affect adherence, it may be a great obstacle to patient who are requiring oxygen or using it. Unwanted attention may interfere with initiation of portable OT, and fear of permanent use may make patients hesitate to initiate home OT. Restriction of daily activities will weigh on the patients with emotional burden. Identifying unrecognized perceptions and helping patients overcome negative perspectives could provide opportunities to improve initiation of OT and to explore what it is like living in a life-limiting condition. Sharing these experiences may help individuals make informed choices regarding advanced care plans for terminal chronic respiratory diseases.
1. Limitations
This study included patients who voluntarily agreed to complete the questionnaire. Therefore, only a small number of participants were enrolled. Nevertheless, our finding is meaningful. While previous studies on LTOT focused on patients who were currently using home or portable OT, the strength of this study is that it included patients who needed LTOT but avoided using it. Second, circumstances that might have influenced the survey results were excluded from the analysis. Underlying respiratory diseases, disease severity, performance status, equipment type, oxygen flow rate, and other confounding factors may have been hidden outside the scope of our survey. Further exploration of these factors may provide more information on patient compliance with LTOT. Despite these limitations, the results of this study can guide future studies aimed at managing and supporting negative perceptions as barriers to LTOT.
2. Conclusion
This study examined the perceptions of patients currently using or avoiding LTOT in Korea. Although the use of portable oxygen devices has increased since the insurance coverage was extended, patients’ compliance remains poor. An important difference was the perception of the effects of OT between patients with good and poor compliance. The psychosocial barriers that the patients in both good and poor adherence groups may be a great obstacle to patient who are requiring oxygen or using it. Considering these findings, health professionals need to provide effective education on the purpose of LTOT to improve patient adherence to OT and provide sufficient support for the management of psychosocial barriers in patients using LTOT.
Notes
Authors’ Contributions
Conceptualization: Lee H, Lee HK. Methodology: Yang JY, Lee HK. Formal analysis: Kim HJ, Lee H, Hong SM. Data curation: Lee H, Lee JH, Ra SW, Lee HY, Kim SH, Kim MY, Lee HK. Investigation: Kim HJ, Lee H. Writing - original draft preparation: Kim HJ, Lee H. Approval of final manuscript: all authors.
Conflicts of Interest
Seung Won Ra is an editorial board member of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Funding
No funding to declare.
Supplementary Material
Supplementary material can be found in the journal homepage (http://www.e-trd.org).
The reasons for reluctance to use LTOT in all enrolled patients



