Invasive Aspergillosis Involving the Lungs and Brain after Short Period of Steroid Injection: A Case Report
Article information
Abstract
Invasive pulmonary aspergillosis (IPA) has emerged as a severe infection in patients with immunocompromised hosts. However, recently, several IPA cases, without an apparent predisposition to immunodeficiency, has been reported. A 72-year-old woman was admitted for evaluation of general weakness and poor oral intake. She reported no medical history, except for intraarticular injection of a corticosteroid for joint pain for the duration of two months. A chest radiography revealed multiple cavitary nodules in both lungs. Examination of specimens, obtained by percutaneous needle biopsy, led to a diagnosis of invasive aspergillosis. Brain magnetic resonance imagining revealed numerous peripheral thin enhancing cystic nodules in both cerebral hemispheres. We initiated intravenous administration of amphotercin B. However, the patient died after nine days. Here, we report an invasive aspergillosis case, which involves the lungs and brain after a short period of steroid injection.
Introduction
Aspergillosis is a disease caused by fungi of the genus Aspergillus. The most common clinical manifestations are allergic bronchopulmonary aspergillosis, pulmonary aspergilloma and invasive aspergillosis1.
Aspergillus species are frequently found in surrounding environment such as soil, food and water, and their spores are frequently aerosolized by air. Although exposure to the organism is frequent, invasive infections most often occur almost in immunocompromised hosts such as neutropenic patients with hematologic malignancies, solid organ transplant recipients who have undergone immunosuppressive treatment, and hemodialysis patients2,3. These findings suggest a strong relationship between the invasive aspergillus infection and human immunity4.
Generally, cases of invasive aspergillosis in immunecompetent hosts are rare. Here, we report invasive aspergillosis case involving the lungs and brain involvement after a short period of steroid injection.
Case Report
A 72-year-old woman was admitted to the hospital for general weakness and poor oral intake of a two-week duration. The patient experienced bilateral knee joint pain on walking, and the symptoms had exacerbated since 4 months. She visited a local orthopedic hospital 2 months ago and was diagnosed with osteoarthritis by simple X-ray analysis, she started receiving intra-articular steroid injections. Triamcinolone acetonide (Kenalog-40), which is typically used for large joints, was used a total dose of 80 mg once a week for 2 months on both sides of the knee joints. She did not undergo glucose monitoring during this period. The pain in both knee joints reduced during treatment. In 2004, she underwent cholecystectomy our hospital; the random glucose level was normal during that period, and she did not have typical symptoms of diabetes and cushing's syndrome. While undergoing orthopediatric treatment, she had weight gain associated with mild systemic edema, which may have been related to cushing's syndrome, the symptoms had progressive pattern.
On admission, her vital signs were as follows: blood pressure, 120/80 mm Hg; pulse, 98 beats per minute; respiratory rate, 20 breaths per minute; and body temperature, 37.9℃. Physical examination revealed acute ill appearance on the face. In addition, she was constantly sleepy and had multiple ulcers with whitish patches in the oral mucosa. Chest auscultation revealed a mild crackle sound in the entire lung field. Other results of the physical examination were non-specific.
Her blood examination showed a hemoglobin level of 15.3 g/dL, white blood cell count of 13×103/mL (neutrophils, 96.3%; lymphocytes, 3.1%; and monocytes, 0.6%), and platelet count of 349×103/µL. The biochemical profile showed mild hyperglycemia (random blood glucose level, 174 mg/dL), and a Hb A1C level of 7.7%. The levels of fasting plasma C-peptide, serum albumin, and C-reactive protein were 6.1 ng/mL, 2.4 g/dL, and 13.37 mg/dL, respectively. The human immunodeficiency virus test was also negative. Other biochemical profiles were within the normal range. The results of the thyroid function test were as follows: T3 level, 10 ng/dL (normal range, 60~90 ng/dL), free T4 level, 1.2 ng/dL (normal range, 0.89~1.79 ng/dL), thyroid stimulating hormone level, 30 mIU/mL (normal range, 170~405 mIU/mL). These findings suggested a sick euthyroid state. Because of her severe general weakness, we performed the rapid adrenocorticotropic hormone stimulation test for the evaluation of adrenal function. The basal cortisol level was found to be 0.55 µg/dL, the 30 minute cortisol level was 6.3µg/dL and the 90 minute cortisol level was 5.5µg/dL. These findings were compatible with adrenal insufficiency.
The chest X-ray film revealed multiple cavitary nodules in both lungs (Figure 1). Chest computed tomography scan revealed mass and cavitary nodules with mild homogenous enhancement in both lungs (Figure 2).

Chest X-ray findings. (A) At admission. Chest X-ray revealed multiple cavitary nodules in both lungs. (B) At hospital 6 days. Chest X-ray revealed aggravating state of nodules and haziness in both lungs.
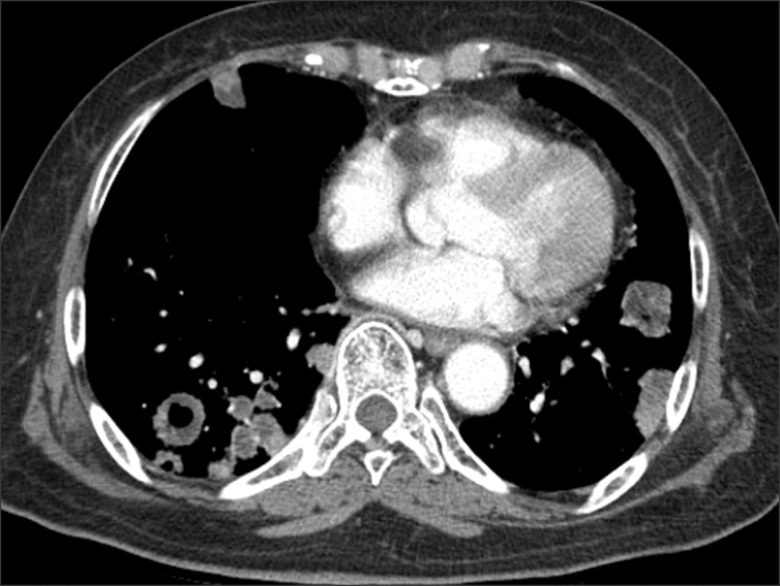
Chest computed tomography (CT) findings. Chest CT revealed multiple cavitary nodules and masses in both lungs.
On the third hospital day, percutaneous needle biopsy was performed for differential diagnosis of malignant metastasis and rare diseases such as fungus, vasculitis. Biopsy shows an aggregate of fungal hypae with acute angle branching and a rare fruit body (Figure 3).
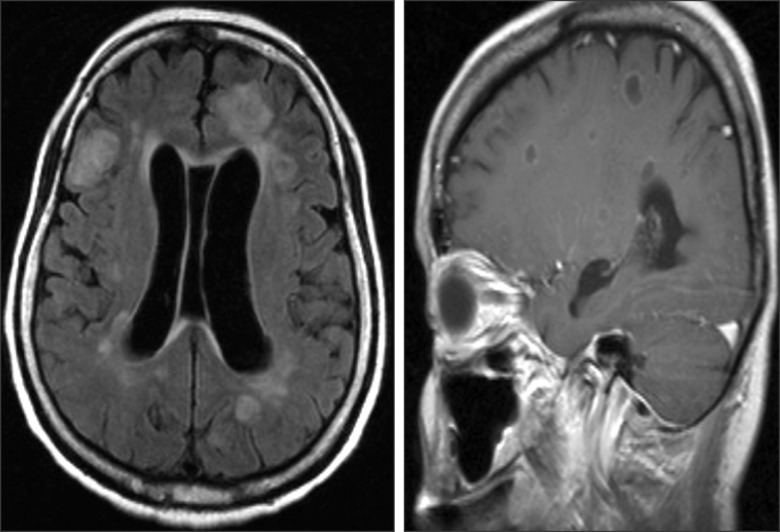
Brain magnetic resonance imaging (MRI) findings. Brain MRI revealed numerous peripheral thin enhancing cystic nodules in right and left cerebral hemispheres.
Hence, we diagnosed her condition as invasive aspergillosis involving the lungs. We thought that risk factor for invasive aspergillosis was diabetes caused by the intraarticular corticosteroid injection.
On the fifth hospital day, we intravenously administered amphotericin B. However, on the sixth hospital day, she became unconscious, hence, we performed a brain magnetic resonance imaging (MRI) and conducted cerebrospinal fluid (CSF) tapping. The MRI showed numerous thin peripheral enhancing cystic nodules at bilateral cerebral hemispheres (mainly cortex and subcortical white matter), basal ganglia, pons, and midbrain (Figure 4). CSF examination showed non-specific findings. We concluded that the brain was also involved by invasive aspergillosis, and we continued intravenous amphotericin B treatment, but her condition deteriorated daily.

Histologic finding shows an aggregate of fungal hypae with acute angle branching and rare fruiting body (GMS stain, ×400).
On the eighth hospital day, she was transferred to the intensive care unit for ventilator care, and treatment with amphotericin B was replaced with voriconazole. However her condition kept deteriorating every day. On the 14th hospital day, she died from respiratory failure and septic shock.
Discussion
The Aspergillus species are frequently found in surrounding environment, and commonly affect patients receiving chemotherapy, solid organ transplant, and allogeneic stem cell transplant4,5.
However recently, several reports have described the emergence of atypical patient group at risk for invasive aspergillosis; this group included intensive care unit patients, those with chronic respiratory disorders, and post-operative patients3.
We speculate that our patient had an increased susceptibility to infections because of the intraarticular corticosteroid injection therapy. Corticosteroids significantly affect the function of neutrophils and lymphocytes and directly stimulate the growth of Aspergillus5.
The mortality rate in such atypical patient groups is as high as almost 20%. Therefore, an early diagnosis is very important, nevertheless, correct and early diagnosis is difficult because of non-specific clinical symptoms, signs and lack of clear diagnostic criteria of invasive aspergillosis.
Hence, for the diagnosis of such cases, we must consider a multidirectional approach that includes information on the radiologic findings, pathologic findings, and host's immune state.
In most cases of cerebral aspergillosis, the primary site of infection was the lungs, and such cases usually have a poor prognosis. New antifungal therapies involving drugs such as voriconazole are effective in the treatment of cerebral aspergillosis because of their good penetration to brain3. Herbrecht et al.6 studied invasive aspergillosis and reported that the survival rate in the voriconazole treated group (70.8%) was higher than that in the amphotericin B treated group (57.9%) at 12 weeks.
Therefore, in suspected cases of invasive aspergillosis, concurrent diagnosis procedures and treatments such as voriconazole should be considered as initial therapy7.
In our patient, diagnosis of invasive aspergillosis was delayed, because she had not previously specified her medical history except intra-articular corticosteroid injection therapy. Therefore, we thought her condition to metastatic cancer as an initial diagnosis, and hence, the treatment with antifungal agents was delayed. After the lung biopsy, we diagnosed her condition as invasive aspergillosis on fifth hospital day and started the amphotericin B therapy. The Korean healthcare system has recommended the amphotericin B as the initial treatment for most invasive aspergillosis cases.
In addition to the other ailments, our patient also suffered from adrenal insufficiency and hyperglycemia due to the corticosteroid injections. All these together led to rapid worsening of her condition and finally, death.
Triamcinolone acetonide reversibly suppresses the hypothalamic-pituitary-adrenal axis, this usually occurs within 24~48 hours of administering the drug and is gradually within approximately 30~40 days8,9. To prevent these adverse effects during the treatment, glucose monitoring and dose reduction should be considered, depending on the exact symptoms. Similar to systemic administration, Intra-articular administration of steroids can also cause glucose intolerance9. Pediatric cases of Cushing's syndrome caused by intra-articular injection of triamcinolone acetonide have been reported10.
From the experience with this case, we learned that invasive aspergillosis can be occured in patients without previous immunological disorders. Also, we learned that we should keep in mind the importance of early diagnosis, early treatment, and optimal antifungal treatment in suspected invasive aspergillosis case.