Altered Thoracic Cage Dimensions in Patients with Chronic Obstructive Pulmonary Disease
Article information
Abstract
Background
Chronic obstructive pulmonary disease (COPD) may cause changes in the shape of the thoracic cage by increasing lung volume and hyperinflation. This study investigated changes in thoracic cage dimensions and related factors in patients with COPD.
Methods
We enrolled 85 patients with COPD (76 males, 9 females; mean age, 70.6±7.1 years) and 30 normal controls. Thoracic cage dimensions were measured using chest computed tomography at levels 3, 6, and 9 of the thoracic spine. We measured the maximal transverse diameter, mid-sagittal anteroposterior (AP) diameter, and maximal AP diameter of the right and left hemithorax.
Results
The average AP diameter was significantly greater in patients with COPD compared with normal controls (13.1±2.8 cm vs. 12.2±1.13 cm, respectively; p=0.001). The ratio of AP/transverse diameter of the thoracic cage was also significantly greater in patients with COPD compared with normal controls (0.66±0.061 vs. 0.61±0.86; p=0.002). In COPD patients, the AP diameter of the thoracic cage was positively correlated with body mass index (BMI) and 6-minute walk test distance (r=0.395, p<0.001 and r=0.238, p=0.028) and negatively correlated with increasing age (r=−0.231, p=0.034). Multiple regression analysis revealed independent correlation only between BMI and increased ratio of AP/transverse diameter of the thoracic cage (p<0.001).
Conclusion
Patients with COPD exhibited an increased AP diameter of the thoracic cage compared with normal controls. BMI was associated with increased AP diameter in these patients.
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by progressive, incompletely reversible airflow obstruction, and enhanced chronic inflammatory responses to noxious particles or gases in the airways and lungs1. In a significant proportion of patients with COPD, reduced lung elastic recoil combined with expiratory flow limitation eventually leads to lung hyperinflation with progression of disease2. Increased lung volume and hyperinflation may cause changes in the shape of the thoracic cage in COPD patients. Therefore, it has been traditionally accepted that COPD patients exhibit increased thoracic cage dimensions, especially anteroposterior (AP) diameter, leading to a circular, “barrel-chest” appearance due to increased lung volume and hyperinflation345678.
Despite these findings, previous investigations examining changes in the thoracic cage of COPD patients have reported varying results. Studies measuring the diameter of the thorax have reported no differences in terms of total lung capacity (TLC) and residual volume (RV) between patients with emphysema and healthy subjects89. Other studies have reported an increase in the AP diameter of the thorax in patients with COPD compared with normal subjects, especially in the lower part of the thoracic cage, when examined at the level of functional residual capacity10. We hypothesized that because changes in the shape of the thoracic cage in the normal population can be affected by various factors such as height, weight, age and sex111213, these changes in COPD patients may be more complex than initially believed.
The primary objective of this study, therefore, was to evaluate changes and differences in thoracic cage dimensions of patients with COPD compared with normal controls using chest computed tomography. Our secondary objective was to investigate the factors associated with changes in thoracic cage dimensions in patients with COPD.
Materials and methods
1. Study population and data collection
Patients with stable COPD, who visited the department of outpatient pulmonology, were reviewed. COPD was defined as incompletely reversible airflow, and post-bronchodilator forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) ratio <0.7 in patients with symptoms including dyspnea, cough, and productive sputum. The severity of COPD was classified according to post-bronchodilator FEV1, based on the spirometric guidelines of the Global Initiative for Chronic Obstructive Lung Disease (GOLD)1: stage 1 (FEV1 ≥80%), stage 2 (50%≤FEV1<80%), stage 3 (30%≤FEV1<50%), and stage 4 (FEV1<30% or FEV1≤50% plus chronic respiratory failure). Patients with underlying lung disease, such as bronchiectasislung cancer, interstitial lung disease and fibrothorax, and those with co-existing deformity of the thoracic cage were excluded. The normal control group comprised individuals who visited general health clinics and underwent a chest computed tomography (CT) scan and had normal spirometry results. Age- and sex-matched healthy individuals were enrolled as normal controls. Body mass index (BMI)-matched control subjects were recruited because of the influence of height and weight on thoracic cage dimensions. Individuals in the control group with any history of lung disease were excluded.
Clinical characteristics and demographic data, including smoking history and pulmonary function, were retrospectively collected by chart review. Given the retrospective nature of the study and the use of anonymized data, requirements for informed consent were waived. This study was approved by the Institutional Review Board of the Gyeongsang National University Changwon Hospital (GNUCH-2017-09-002).
2. Pulmonary function testing and 6-minute walk test distance
Spirometric testing was performed in accordance with criteria published by the American Thoracic Society and the European Respiratory Society14. FEV1 and FVC were calculated from the flow-volume curve using a spirometer (Jaeger, Würzburg, Germany). The highest value from at least three independent measurements was recorded. Lung function parameters were expressed as a percentage of the reference values. Exercise performance was based on a standardized protocol and measured using the distance covered in the 6-minute walk test (6-MWT)15.
3. Measurement of thoracic cage dimensions using chest CT
Thoracic cage diameters were measured using chest CT and a modified method based on a previous report16. Thoracic cage diameters were measured it at three anatomical levels (thoracic vertebrae level 3, 6, and 9) because measurement at one anatomical level may result in error(s). The measurements were performed by one professor of the diagnostic radiology department, who performed three measurements at different times at each thoracic level and averaged the data. For each thoracic segment, several thoracic cage diameters were measured using an electronic caliper at CT scan. The maximal transverse diameter (A), mid-sagittal AP diameter (B), the maximal AP diameter of the right (C), and left hemithorax (D) were measured (Figure 1).
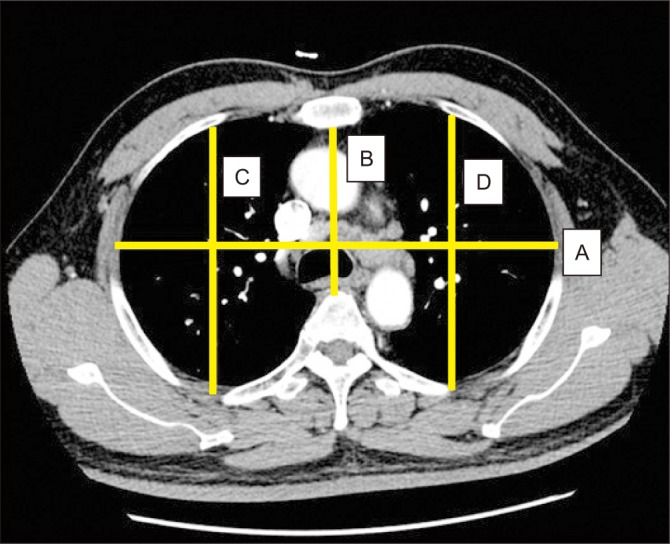
Example illustrating the thoracic cage dimensions. A, the maximal transverse diameter (from the most external midpoint of the rib of one side to the opposite one); B, mid-sagittal anteroposterior diameter (from the inner surface of the sternum to ventral surface of the vertebral body); C and D, the maximal anteroposterior diameters of the right and left hemithorax (from the ventral-most point to the dorsal-most point of the rib cage in each hemithorax).
4. Statistical analysis
The data are presented as mean±standard deviation or as number (%). Continuous variables and categorical variables were compared using an unpaired t test, and the groups were compared using Pearson's chi-square test. Pearson correlation analysis was performed to evaluate relationships between clinical parameters, pulmonary function, and thoracic cage diameter; p<0.05 was considered to be statistically significant for all tests. Univariate and multivariate linear or logistic regression analyses were performed to evaluate factors associated with change(s) in thoracic cage dimensions. Factors found to be significant at the p<0.2 level in the univariate analysis, and factors considered to be significant were subjected to backward-step linear or logistic multivariate analysis. Values that reached a p<0.05 level of significance were considered to be significant. All statistical analyses were performed using SPSS version 22.0 (IBM Corp., Armonk, NY, USA) for Windows (Microsoft Corporation, Redmond, WA, USA).
Results
1. Baseline characteristics of COPD patients and normal controls
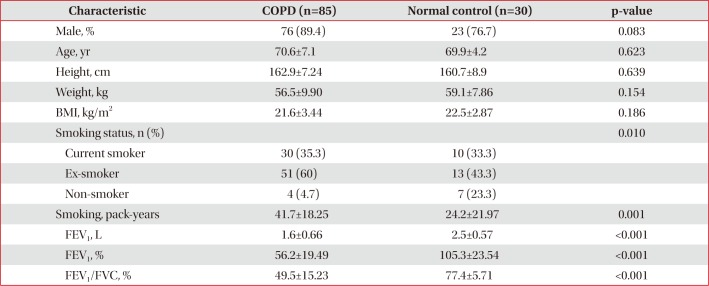
The basic characteristics of patients with COPD and controls are summarized in Table 1. Eighty-five patients (76 male, 9 female; mean age, 70.6±7.1 years) with COPD, and 30 individuals (23 male, 7 female; mean age, 69.9±4.2 years) with normal lung function (control group) were included in this study. There were no significant differences in male ratio, age, weight, height, or BMI between COPD patients and controls. The proportion of non-smokers was higher in controls than in the COPD group. The mean FEV1 in COPD patients was 56.2%, which was approximately one-half of the value in controls.
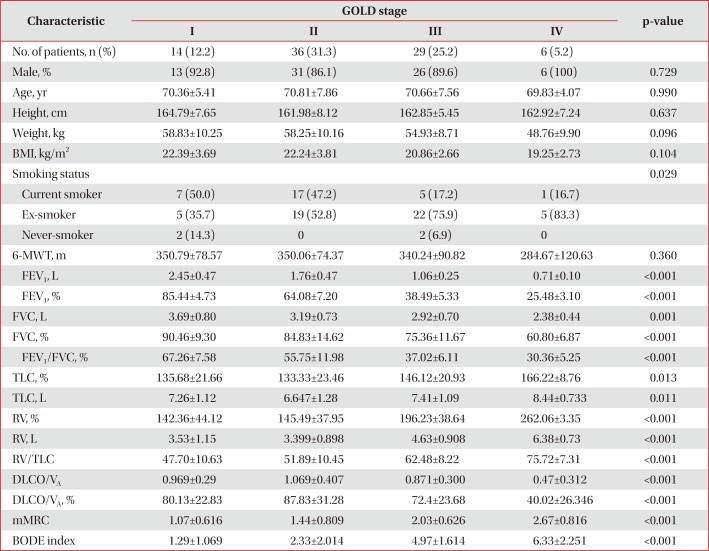
Most patients with COPD were categorized as GOLD stage 2 (n=36, 31.3%) and GOLD stage 3 (n=29, 25.2%). There were no differences in the proportion of males, age, BMI, and 6-MWT distance according to COPD GOLD stage. The proportion of current and ex-smokers was higher in GOLD stage I and II than in GOLD stages III and IV. Pulmonary function tests, such as FEV1, FVC, FEV1/FVC, TLC, RV, and diffusing capacity for carbon monoxide, were significantly different according to GOLD stage. In addition, the modified Medical Research Council and Body-Mass Index, Airflow Obstruction, Dyspnea, and Exercise (BODE) indexes were also significantly different according to GOLD stage (Table 2).
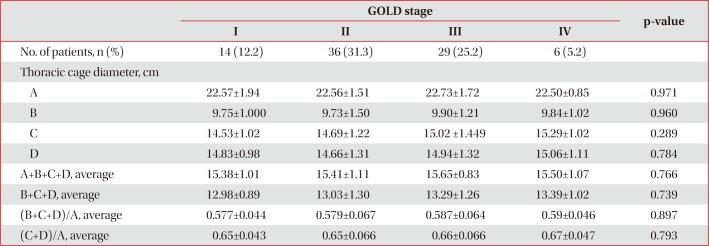
2. Comparison of thoracic cage dimensions in COPD patients and normal controls
A comparison of thoracic cage dimensions between COPD patients and normal controls is presented in Table 3. The average AP diameter of the right (C) and left hemithorax (D) were significantly greater in COPD patients than in controls (14.79±1.27, 14.81±1.24 cm vs. 13.11±2.620, 14.05±1.25 cm, respectively). Average thoracic AP (B+C+D) diameter in the COPD group was significantly greater than in the control group (13.14±1.20 cm vs. 12.25±1.13 cm, respectively). The ratio of average AP and transverse diameter was also significantly greater in COPD patients than in controls (0.58±0.06 vs. 0.55±0.06, respectively). However, the average maximal transverse diameter (A) and mid-sagittal AP diameter (B) was not different between the COPD and control groups. According to GOLD stage, the transverse and AP diameters were not significantly different (Table 4). The ratio of average AP and transverse diameter was also different in COPD patients according to GOLD stage.
3. Relationship between changes in thoracic cage dimensions and clinical parameters in COPD patients
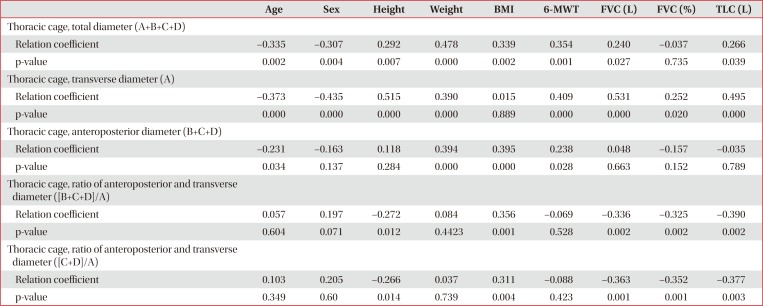
In COPD patients, the total diameter of the thoracic cage was positively correlated with height, weight, BMI, 6-MWT, FVC (L), and TLC (L). Age was inversely correlated with total diameter of the thoracic cage in COPD patients (r=−0.335, p=0.002). The transverse diameter in COPD patients was positively correlated with height, weight, 6-MWT, FVC (L), and TLC (L), but not BMI. Age was inversely correlated with transverse diameter in COPD patients (r=−0.373, p<0.001). The AP diameter in COPD patients was positively correlated with weight, BMI, and 6-MWT, but not FVC (L) or TLC (L). Age was also inversely correlated with AP diameter in COPD patients (r=−0.231, p=0.034). The ratio of AP and transverse diameter in COPD patients was positively correlated with height, BMI, FVC (L), and TLC (L), but not 6-MWT distance. Age was not related to this ratio in COPD patients (Table 5).
4. Factors related to increased ratio of AP and transverse dimeter of the thoracic cage in patients with COPD
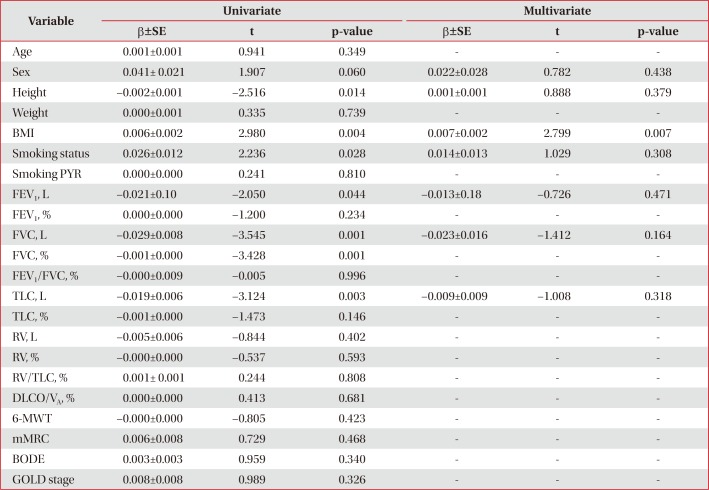
Table 6 summarizes the results of the univariate and multivariate regression analysis for factors related to increased ratio of AP and transverse diameter of the thoracic cage in patients with COPD. In univariate analysis, height, BMI and smoking status were significantly associated with increased ratio of AP and transverse diameter of the thoracic cage in patients with COPD. Spirometric values of FEV1 (L), FVC (L), FVC (%), and TLC (L) also demonstrated a significant association. In multivariate analysis, an increased ratio of AP and transverse diameter of the thoracic cage was associated only with BMI in COPD patients (p=0.007).
Discussion
This study revealed an increased AP–but not transverse–diameter of the thoracic cage in COPD patients compared with normal controls, and BMI was significantly associated with changes in thoracic cage dimensions of COPD patients.
The finding of increased AP diameter of the thoracic cage in COPD patients is consistent with results reported in previous studies912171819202122. However, as a measurement method, we consider that the use of CT in our study was more accurate than the simple caliper measurement of the chest wall and chest X-ray reported in previous studies162122.
If changes in the thoracic cage are reflective of the degree of hyperinflation, which is associated with more severe airflow obstruction, it is generally a more structural change in patients with COPD. However, the AP diameter of the thoracic cage did not exhibit a difference according to the severity of COPD in our study. In addition, increased lung volume, which was assessed using TLC and RV in this study, was not associated with increased AP diameter of the thoracic cage. These results suggest that thoracic cage changes in COPD may be associated with not only the degree of hyperinflation and lung function decline, but also various other factors including age, sex, weight, and height.
Age is an important factor in changes of the thoracic cage in the normal population. The elderly population typically exhibits a narrowing of the intervertebral disk space, which causes curvature of the spine, known as kyphosis23. This curvature decreases intercostal space and eventually leads to a smaller thoracic cage24. In this study, we also demonstrated that the overall diameter of the thoracic cage decreases with increasing age and rounding of the thoracic spine, resulting in greater decreases in AP diameter than the transverse diameter. Because COPD is more prevalent in elderly individuals25, age-related changes in the thoracic cage are considered to be important contributing factors in these patients.
It is also known that there are sex-related differences in the shape of the thoracic cage. Previous studies investigating factors associated with changes in the shape of the thoracic cage have reported that sex has a greater influence on thoracic cage diameter than other factors such as BMI or age16. It is generally known that the size of the thoracic cage in women is approximately 10% to 20% smaller than that of men, which is primarily related to the reduction of AP diameter of the thoracic cage112627. The proportion of males in the COPD group was not higher than in the normal controls in our study. Moreover, sex did not appear to be related to increased AP diameter in univariate and multivariate regression analysis in COPD patients. Therefore, our results suggest that sex-related factors may be not associated increased AP diameter in COPD patients.
BMI is also associated with the shape of the thoracic cage121628. In this study, BMI was independently associated with increased AP diameter and the ratio of AP/transverse diameter of the thoracic cage in COPD patients. We encountered limitations in studying the relationship between BMI and thoracic cage dimension in COPD patients. A previous study reported that increasing BMI may increase thoracic cage diameter in patients with emphysema, especially in the lower part of the lungs16. As a general concept, increased BMI can increase total thoracic cage length, which increases the AP diameter of thoracic cage. In this study, BMI was associated with increased the ratio of AP/transverse diameter, and our results demonstrate that height and weight have different effects on thoracic cage dimensions. This study revealed that height is more strongly associated with transverse–not AP–diameter of the thoracic cage. In contrast, weight is more strongly associated with AP–not transverse–diameter of the thoracic cage. We speculate that because BMI may be more influenced by weight than height, increased BMI was associated with increased AP diameter and the ratio of AP/transverse diameter of the thoracic cage in COPD patients.
Although a relationship between increased thoracic cage diameter in COPD patients and lung volume was not documented in this study, several studies have reported changes in thoracic cage diameter according to lung volume. Salito et al. measured rib-cage diameter in five patients with severe emphysema using CT. They reported that the AP diameter of the rib-cage was greater in COPD patients than in controls according to RV, but not TLC29. Lung volume reduction surgery also may reduce AP rib-cage diameter in patients with severe COPD7. We believe that it is necessary to evaluate these relationships in more patients with severe COPD and hyperinflation, and to assess the degree of hyperinflation than simple lung volume.
We expected increased thoracic cage diameter to be associated with reduced exercise capacity in COPD patients because increased thoracic diameter may reflect more severe illness. However, the results of this study suggested that increased AP diameter of thoracic cage was positively associated with increased exercise capacity. This is because subjects with higher BMI usually exhibit better exercise performance than those with COPD30. BMI has a greater effect on exercise capacity than thoracic cage diameter. In addition, exercise capacity in COPD patients is known to be associated not only with lung function but also various other factors, such as cardiac function, ventilator demand, and weakening and atrophy of peripheral skeletal muscles3132.
This study had some limitations, the first of which was its retrospective design. Second, we enrolled patients who underwent chest CT scan and 6-MWT. Therefore, the number of patients with severe COPD was limited because those with more severe COPD are often unable to perform exercise tests because of dyspnea. In addition, clinical characteristics, such as the degree of emphysema, frequency of exacerbation, and the phenotype of COPD associated with change(s) in the thoracic cage did not investigated in this study.
In conclusion, this study demonstrated that AP diameter of thoracic cage, measured using CT, was increased in COPD patients compared with normal controls. BMI was the only factor associated with increased AP diameter of the thoracic cage in COPD patients. Additional factors related to changes in the thoracic cage as COPD progresses will be investigated in the future.
Notes
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.