Comparison of Multiple Chronic Obstructive Pulmonary Disease (COPD) Indices in Chinese COPD Patients
Article information
Abstract
Background
Chronic obstructive pulmonary disease (COPD) is a serious chronic condition with a global impact. Symptoms of COPD include progressive dyspnea, breathlessness, cough, and sputum production, which have a considerable impact on the lives of patients. In addition to the human cost of living with COPD and the resulting death, COPD entails a huge economic burden on the Chinese population, with patients spending up to one-third of the average family income on COPD management in some regions is clinically beneficial to adopt preventable measures via prudent COPD care utilization, monetary costs, and hospitalizations.
Methods
Toward this end, this study compared the relative effectiveness of six indices in predicting patient healthcare utilization, cost of care, and patient health outcome. The six assessment systems evaluated included the three multidimensional Body mass index, Obstruction, Dyspnea, Exercise capacity index, Dyspnea, Obstruction, Smoking, Exacerbation (DOSE) index, and COPD Assessment Test index, or the unidimensional measures that best predict the future of patient healthcare utilization, cost of care, and patient health outcome among Chinese COPD patients.
Results
Multiple linear regression models were created for each healthcare utilization, cost, and outcome including a single COPD index and the same group of demographic variables for each of the outcomes.
Conclusion
We conclude that the DOSE index facilitates the prediction of patient healthcare utilization, disease expenditure, and negative clinical outcomes. Our study indicates that the DOSE index has a potential role beyond clinical predictions.
Introduction
Chronic obstructive pulmonary disease (COPD) is a serious chronic condition which has a global impact. Symptoms of COPD include progressive dyspnea, breathlessness, cough, and sputum production, which can have a considerable impact on the lives of the patients experiencing it1. The impact of COPD on the population in China is significant, with a recent estimate placing the prevalence rate at 8.2%2 with a mortality rate of approximately 1.6%3. In addition to the human costs, COPD places a high economic burden on the Chinese population, with patients spending up to one-third of the average family income on COPD management costs in some regions3. Given morbidity and mortality that COPD can pose on people's lives, yet the difficulty of detection in cases with mild symptoms that become rapidly worse, simple yet comprehensive prediction tools are highly useful. These could be clinically and managerially beneficial in predicting COPD care utilizations, monetary costs, and hospitalizations that are preventable.
Multiple tests have been devised for these purposes. This study compared the relative effectiveness of these six indices in predicting patient healthcare utilization, cost of care, and patient health outcome. The indices used for this study are as follows: the Body mass index, Obstruction, Dyspnea, Exercise capacity (BODE) index which was the first multidimensional assessment for COPD4, the Dyspnea, Obstruction, Smoking, Exacerbation (DOSE) index5, and the COPD Assessment Test (CAT)6 as well as the unidimensional modified Medical Research Council (mMRC) Dyspnea Scale7, the derived forced expiratory volume in 1 second predicted (FEV1%pred) value8, and the 6-minute walk test (6MWT)9. The primary goal of the present study, was to identify which of the six assessment systems, the three multidimensional the BODE, DOSE, or CAT indices, or the unidimensional three measures best predicts the future patient healthcare utilization, cost of care, and patient health outcome among Chinese COPD patients. The results of this study could help clinicians and hospital administrators to manage this chronical disease early and efficiently and therefore avoid unnecessary adverse events and costs.
Materials and methods
1. Sample and data collection
This longitudinal study followed participants over the course of a year. All patients who were treated inpatient or outpatient for acute exacerbation of COPD in the Department of Respiratory Medicine between December 2013 and December 2014 were selected for the study. Three hundred and fifty patients who met the Global Initiative for Chronic Obstructive Lung Disease diagnostic criteria of COPD10 from The Second Affiliated Hospital of Kunming Medical University were initially included in the study. The Second Affiliated Hospital of Kunming Medical University provided ethics approval for exempted informed consent. Exclusion criteria included those with left ventricular failure, neuropsychiatric disorders, cancer, immune deficiency, renal failure, chronic liver disease, malignant tumors, and those who opted out of the study. The presence of any these conditions excluded them form consideration in the study. The number of patients who remained in the study for the year was 129; meaning that 221 patients were either excluded or dropped out of the study over the year. Data were collected through medical chart review and self-administered questionnaires. Information on patient outpatient and emergency room (ER) visits, costs, and inpatient stays were retrieved from electronic medical record by pulmonologists. Between December 2013 and December 2014 the patients were also mailed self-completed questionnaires. Participants were asked questions regarding disease severity, the number of exacerbations, the results of 6MWT, the mMRC Dyspnea Scale, and the FEV1%pred value. Participants were followed up before and after the study period and methods such as random visit and multiple locations (home, hospital, etc.) and utilized a variety of communication means (telephone, interviews, etc.).
2. Multidimensional measures
1) The BODE index
The BODE index is calculated using the FEV1%pred, the 6MWT, mMRC Dyspnea Scale, and the body mass index of the patient. The BODE index uses the sum of its components and the total score ranges from 0 to 10 points. The higher the score, the higher predicted fatality over the next 4 years.
2) The DOSE index
The DOSE index is calculated using the mMRC Dyspnea Scale, FEV1%pred, smoking status, and the exacerbation rate in the previous year. The DOSE index uses the sum of its components and the total score ranges from 0 to 8; the higher the score, the more severe the disease.
3) CAT index
The CAT is calculated using patient reported answers to eight 5-point Likert scale questions. The total score ranges 0–40. The CAT, in relation to physiological tests can be indicative of disease severity, with a higher score meaning more severe disease.
4) Healthcare utilization
The factors which were used to determine healthcare utilization were the length of stay at the hospital, number of hospitalizations, number of ER visits, and number of outpatient visits. These were determined by chart review over the course of the study.
5) Cost of disease burden
The factors which were used to determine healthcare utilization were the costs spent on the self-reported money spent on inpatient costs, ER costs, and outpatient costs over the course of the study.
6) Clinical outcomes
For the purpose of this study, the clinical outcomes of interest were reported cases of heart failure, reported cases of respiratory failure, and cases of self-reported acute deterioration.
3. Statistical analysis
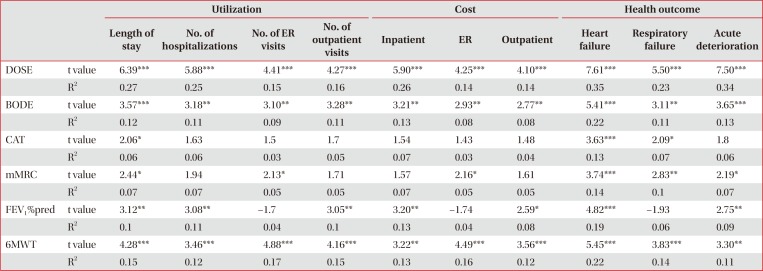
Multiple linear regression models were run on each healthcare utilization, cost and outcome where each COPD index served as the dependent variable and the same group of demographic variables were included for each of the respective outcomes. This means that there were six separate regressions run for each Tables 1, 2 and 3, in order to ensure that indices which were correlated with each other were not within the same analysis. In order to calculate COPD severity changes, the initial reported COPD scores of the given indices were subtracted from the final COPD scores from the same indices for a given patient. The resulting difference became the dependent variables for the regressions in Table 3. The relative effectiveness of prediction of COPD are evaluated based on the model fits (R2) and statistical significances of the indices. A better fit model demonstrated a relative higher R2 value and a statistical significant regression coefficient of an index demonstrated a p-value less than 0.05. Both cross-sectional models and different-in-different models were conducted to examine the sensitivity of the predictions.
Results
During the study period 129 individuals remained in the study for both years, resulting in a retention rate of approximately 36.85%. The descriptive statistics can be seen in Table 1. Included on Table 1 are demographic characteristics. It is worth noting that most participants were male, smokers, and ranged in age from 41 to 89, with an average age of 71.5.
As can be seen in Table 2, the BODE index as well as the DOSE index were positively associated with patient healthcare utilization, cost of disease, and negative clinical outcomes. Although both were positively associated, the magnitude of coefficients associated with the DOSE index were larger. Within the construct of healthcare utilization, the coefficients, there are some sizable differences. For example, the coefficient of the length of stay at the hospital was 3.57 days for the BODE index while it was 6.39 days for DOSE index. Similar differences can be seen within the construct of cost of disease, with a coefficient of 3.21 from the BODE index for the self-reported money spent on inpatient costs, contrasted to a coefficient of 5.90 for the DOSE index. All monetary values were measured in Yuans. Currently $1 US dollar is worth approximately 6 1/2 Yuan. Finally, among the Clinical outcomes, the most drastic difference in coefficient can be seen in the cases of self-reported acute deterioration. There were 3.65 reported cases for each increase in the BODE index while there were 7.50 reported acute deterioration cases for the DOSE index. The CAT index was positively associated with an increase of 2.06 days in length of stay for each point increase of the index. CAT increase was also positively associated 3.63 more reported heart failures and 2.09 more reported respiratory failures. It was not significantly related to any other outcomes.
In Table 3, the comparison of the changes over time between the indices was done. Within this analysis, the DOSE index remained significant with most of the outcome measures. Within healthcare utilization, an increase in DOSE was associated with an increase 4.77 in the length of stay at the hospital. An increase in the DOSE index was associated with 4.43 more hospitalizations over time as well as and 3.87 more ER visits. Within cost of disease, an increase in the DOSE index saw an increase in 4.86 in inpatient costs and 3.96 in ER costs. The DOSE index was positively in relation to the difference in clinical outcomes over the course of the study. An increase in the DOSE index was associated with 2.58 more reported heart failures, 2.88 more reported respiratory failures, and 7.15 acute deteriorations. The only significant relationship with the change in outcomes over the course of the study with the BODE index was the positive relationship with self-reported acute deterioration. It was still significant with an increase in the BODE index seeing 2.75 more acute deteriorations. Interestingly, the CAT index was not significantly related directly with outpatient cost, yet it became positively related with the difference in outpatient cost in Table 3. An increase in the CAT index saw an increase of 2.19 Yuan in outpatient spending.
Discussion
The primary finding of this study is that the DOSE index was the best predictors of all COPD outcomes including patient healthcare utilization, cost of the disease, and negative clinical outcomes out of the six indices examined. Previous studies have shown that DOSE is an effective tool in predicting a range of clinical outcomes5, particularly compared to other indices in the United Kingdom, Sweden, and Holland11 as well as mortality among COPD patients12. The DOSE index even stayed significant in most of the categories when comparing the change between the outcomes between the time periods of the study. This is the first study to demonstrate the relative predictability of DOSE index across comprehensive health outcomes among a group of Chinese patients.
This study has added to the literature positing that the DOSE index is more accurate and reliable than BODE13. The modified BODE has been shown to have a significant discriminative property14, indicating that in the future this should be compared directly to the DOSE index. It is also one of the first studies to compare the DOSE and the CAT. Although DOSE appears to be far more effective than CAT, it does confirm previous literature which found that CAT is a cheap and easy method to gauge certain outcomes in patients15. It has also contributed by providing data on the use of the DOSE index, BODE index, and CAT index in the Chinese population.
This study has several limitations. Although this study was a longitudinal study, there was significant drop out from the participants. It is unknown is those patients were different from the participants who remained in the study. This study utilized patients who had received a diagnosis of COPD; however, it is highly likely that there are patients who had comparable COPD symptoms, yet were not included in the study because their status was not known to the researchers.
In our opinion, the DOSE index is suitable for not only to predict clinical outcomes, but also to predict hospital utilization as well as the financial burden of the disease on the patient. It could be a useful instrument to researchers examining multiple aspects of COPD in the lives of patients.
We conclude that the DOSE index is useful in predicting patient healthcare utilization, cost of the disease, and negative clinical outcomes. The DOSE index was a better predictor for all three outcome categories than its individual components or than the BODE index or the CAT index. Our study indicates that the DOSE index has potential use beyond clinical predictions.
Notes
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.