Cutaneous Leukocytoclastic Vasculitis with Gastrointestinal Involvement after Anti-Tuberculosis Treatment
Article information
Cutaneous leukocytoclastic vasculitis (CLV) is a vasculitis involving the small vessels, usually localized to the skin. CLV may be caused by drugs, infection, collagen tissue disease, or malignancy1. Although several reports describe CLV related to anti-tuberculosis medication23, gastrointestinal involvement of CLV after anti-tuberculosis medication has rarely been reported.
A 72-year-old man was transferred to our hospital with prolonged pneumonia and lung abscess. He was treated with treatment with piperacillin/tazobactam and moxifloxacin but developed septic shock. A specimen obtained from a bronchoscopic washing was positive for Mycobacterium tuberculosis by polymerase chain reaction. The patient was started on anti-tuberculosis treatment with isoniazid, rifampin, and ethambutol. After 2 weeks, the patient developed pruritic patches, macules, and papules on his whole body (Figure 1). A skin biopsy revealed vascular infiltration of neutrophils into the dermis without IgA deposition in immunohistochemistry, which was interpreted as vasculitis. The patient complained of abdominal pain and esophagogastroduodenoscopy showed multiple flat erythematous and hemorrhagic changes in the antrum and lower body of the stomach and in the duodenum (Figure 2A). A biopsy from the stomach showed vascular congestion and hemorrhage, with inflammatory changes in the lamina propria (Figure 2B). The autoantibodies were not significantly increased. Anti-tuberculosis treatment was stopped, and the patient was started on methylprednisolone. This treatment relieved his skin lesions, abdominal pain. Follow-up esophagogastroduodenoscopy showed complete disappearance of all mucosal lesions.
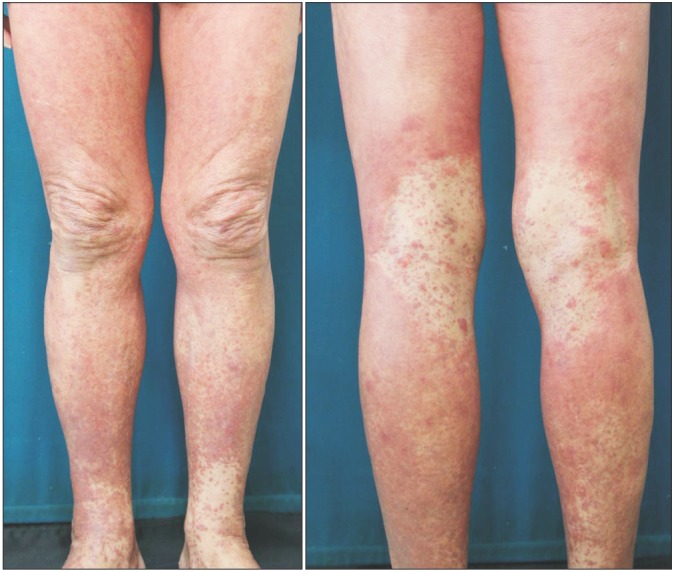
Patient photographs showing the pruritic patches, macules, and papules in both legs extended to the trunk and both arms after 2 weeks of anti-tuberculosis treatment.
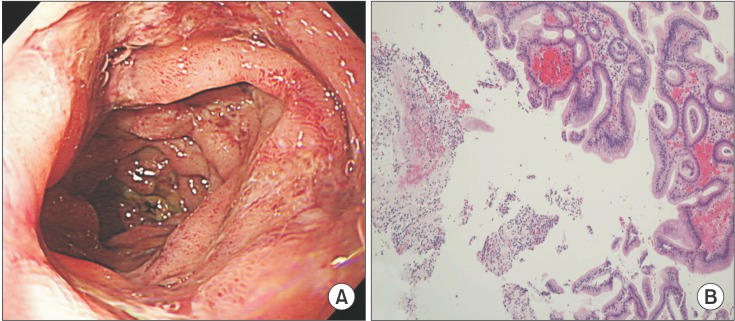
Esophagogastroduodenoscopy of patient showing multiple flat erythematous and hemorrhagic changes in the duodenum at diagnosis (A) and vascular infiltration of neutrophils and hemorrhage in the antrum of the stomach (B) (H&E stain, ×100).
The patient fully met the criteria for CLV, as he was >16 years of age and without arthralgia, renal involvement or IgA deposition in biopsies of the skin and gastrointestinal mucosa45, and did not match the criteria for Henoch-Schönlein purpura or systemic lupus erythematosus. This report described a patient with anti-tuberculosis treatment induced CLV involving both the gastrointestinal tract and skin. Gastrointestinal involvement may occur in patients showing typical features of CLV.
Notes
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.