A Case of Extensive IgG4-Related Disease Presenting as Massive Pleural Effusion, Mediastinal Mass, and Mesenteric Lymphadenopathy in a 16-Year-Old Male
Article information
Abstract
IgG4-related disease is an immune-mediated fibro-inflammatory disease, characterized by lymphoplasmacytic infiltration composed of IgG4-positive plasma cells of various organs with elevated circulating levels of IgG4. This disease is now reported with increasing frequency and usually affects middle-aged men. Massive pleural effusion in children is an uncommon feature in IgG4-related disease. Here, we report a case of a 16-year-old male patient with extensive IgG4-related disease presenting with massive pleural effusion, mediastinal mass, and mesenteric lymphadenopathy.
Introduction
IgG4-related disease is a recently recognized immune-mediated systemic condition that characteristically presents with lymphoplasmacytic infiltrate composed of IgG4-positive plasma cells, storiform fibrosis, obliterative phlebitis, and mild to moderate tissue eosinophilia. This condition is being reported with increasing frequency1. IgG4-related disease can involve almost any organ, including the skin, pericardium, thyroid, prostate, breast, aorta, meninges, lymph nodes, lungs, kidneys, periorbital tissues, salivary glands, biliary tract, and pancreas2. IgG4-related disease frequently affects middle-aged to elderly man3. Massive pleural effusion in children is an uncommon feature in IgG4-related disease.
We report a case of a 16-year-old male patient with extensive IgG4-related disease presenting with massive pleural effusion, mediastinal mass, and mesenteric lymphadenopathy.
Case Report
A 16-year-old male patient was admitted to our hospital complaining of dyspnea and tachypnea. A year ago, he had already been diagnosed with angiomyolipoma through video-assisted thoracoscopic surgery (VATS) mediastinal biopsy. VATS was carried out because mediastinal mass and bilateral loculated pleural effusion was incidently found on health care check-up at school. Preoperative chest computed tomography (CT) scan already showed large amounts of bilateral pleural effusion and anterior mediastinal soft tissue density. But the patient said that he did not accompany symptoms such as dyspnea or tachypnea at that time.
On physical examination, he showed shortness of breath and pitting edema on both legs. The lung sound was diminished on both sides during auscultation of the chest. Routine laboratory tests showed results within normal range. Autoimmune markers such as fluorescent antinuclear antibody and anti-neutrophil cytoplasmic antibody also showed negative results.
A chest radiograph showed bilateral pleural effusion (Figure 1A). Chest CT showed bilateral pleural effusion with loculation, interlobular septal thickening, bronchial wall thickening, and soft tissue density at the anterior mediastinum (Figure 1B-D). Abdomen-pelvic CT showed diffusely increased attenuation of the mesentery and extraperitoneal intra-abdominal fat with a nodular pattern, and also showed enlarged mesenteric lymph nodes. Two-dimensional echocardiography showed normal sized cardiac chambers, preserved left ventricular systolic function, and no significant valvular dysfunction. The characteristics of the pleural fluid showed exudate nature and chylothorax (pleural fluid total protein, 4.2 g/dL; serum total protein, 5.2 g/dL; pleural fluid lactate dehydrogenase (LDH), 213 IU/L; serum LDH, 167 IU/L; pleural fluid triglyceride, 551 mg/dL; pleural fluid carcinoembryonic antigen [CEA], 0.67 ng/mL with no malignant cells; pleural fluid adenosine dehydrogenase [ADA], 10.7 IU/L). The characteristics of the pleural fluid at other hospital before admission at our hospital also showed exudate nature and chylothorax. (pleural fluid total protein, 2.9 g/dL; serum total protein, 4.9 g/dL; pleural fluid LDH, 226 IU/L; serum LDH, 291 IU/L; pleural fluid triglyceride, 286 mg/dL; pleural fluid CEA, <0.5 ng/mL with no malignant cells; pleural fluid ADA, 15 IU/L).
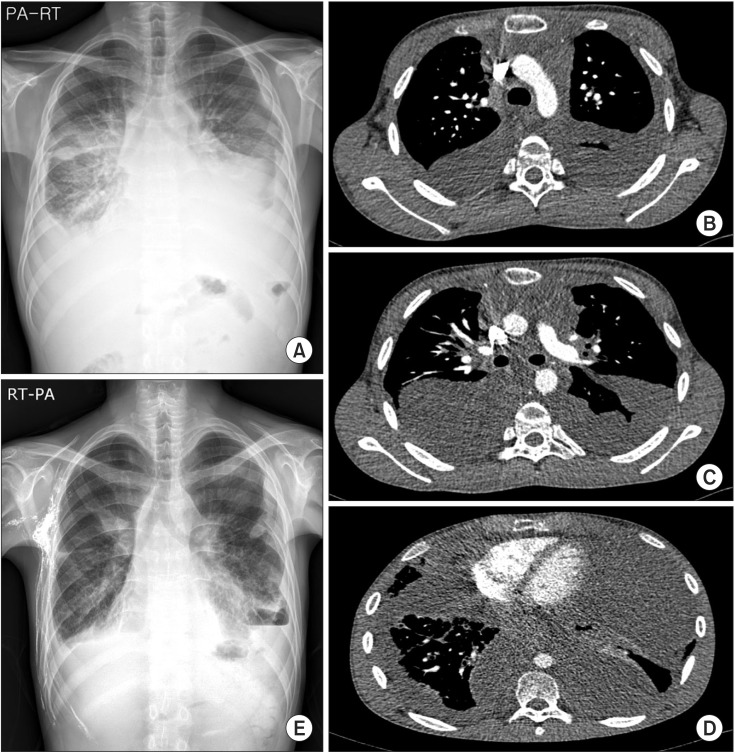
(A-D) Imaging study on admission day showing massive bilateral pleural effusion with loculation, interlobular septal thickening, bronchial wall thickening, and soft tissue density at the anterior mediastinum. (E) A chest X-ray in the posterior-anterior view after 4 months of treatment with systemic steroids and azathioprine showing markedly decreased bilateral pleural effusion. RT-PA, right posterior-anterior view.
The chronic progressive increase of pleural effusion may suggest diffuse pleural involvement of IgG4-related disease. The multiple enlarged mesenteric lymph nodes on abdomenpelvic CT were also suggestive of mesenteric involvement of IgG4-related disease. Our histopathological review of the prior mediastinal biopsy was consistent with IgG4-related sclerosing disease rather than angiomyolipoma, which included papillary proliferation of reactive mesothelial cells and dense collagenous fibrosis with stromal dense lymphoplasmacytic infiltration. The ratio of IgG4- to IgG-positive plasma cells exceeded 40%, and the maximal count of IgG4-positive plasma cells was 62 cells/high-power field (HPF) (Figure 2A-F). In addition, the serum IgG4 level was 1650 mg/dL (normal range, 110-1,570 mg/dL), thereby confirming a diagnosis of IgG4-related disease. In addition, immunohistochemical stains of human melanoma black 45 and melanin-A showed negative results. Therefore, we thought that the previous diagnosis of angiomyolipoma was wrong.
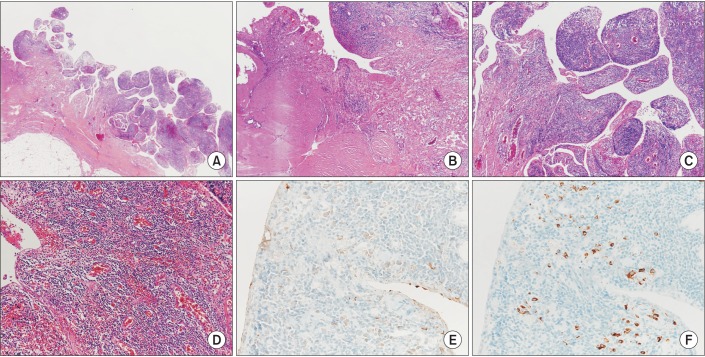
(A-F) Mediastinal biopsy showing papillary proliferation of reactive mesothelial cells and dense collagenous fibrosis with stromal dense lymphoplasmacytic infiltration (IgG4-/IgG-positive plasma cell, >40%; IgG4, maximal count 62/high-power field; human melanoma black 45, negative) (A, H&E stain, ×12.5; B and C, H&E stain, ×40; D, H&E stain, ×100; E, IgG immunostaining, ×200; F, IgG4 immunostaining, ×200).
We started high dose glucocorticoid therapy (prednisolone 1 mg/kg) and drained the pleural effusion by chest tube to relieve the respiratory distress caused by the large amount of pleural effusion. After 2 months of therapy, serum IgG4 level decreased to 450 mg/dL and pleural effusion slightly decreased. But mediastinal mass and mesenteric lymphadenopathies did not show good treatment response. When we reduced the dose of glucocorticoid, pleural effusion and the serum IgG4 level increased. Therefore, we started administration of an oral immunosuppressant (azathioprine) with oral glucocorticoid. A chylorous pleural fluid was continuously drained by chest tube despite treatment with steroid and an oral immunosuppressant (azathioprine). We used octreotide and administrated of limited low fat diet with medium chain triglyceride supplementation, additionally. However, the chylous pleural effusion did not decrease successfully. The patient therefore underwent exploratory thoracotomy and surgical obliteration. After surgical intervention he showed symptomatic improvement and the chest radiograph showed markedly decreased bilateral pleural effusion (Figure 1E).
Discussion
IgG4-related disease is a recently recognized clinical entity caused by an immune mediated-systemic condition that can involve various organs. The observations of Hamano et al.4 have played crucial roles in the identification of this disease. These researchers focused on the fact that several seemingly unrelated diseases shared two characteristics. The first is an elevated serum IgG4 level, and the second is a combination of unique histopathological features, namely a lymphoplasmacytic infiltrates, storiform fibrosis, obliterative phlebitis, and mild to moderate tissue eosinophilia45.
IgG4-related disease can involve various organs, including the salivary glands, thyroid gland, lungs, pancreas, biliary tract, central nervous system, gastrointestinal tract, kidneys, prostate gland, retroperitoneum, and lymph nodes2. In this case, the pleura, mediastinum, and intra-abdominal lymph nodes were involved.
As in our case, biopsy of an involved organ and histopathological confirmation is crucial to diagnose IgG4-related disease. The consensus statement described three major histopathological features: dense lymphoplasmacytic infiltrates, fibrosis arranged at least focally in a storiform pattern, and obliterative phlebitis. At least two of the three major histological features are required for a confident pathological diagnosis1. The absolute IgG4-positive plasma cell counts and the ratio of IgG4- to IgG-positive plasma cells in tissue are considered important secondary diagnostic features to the histopathological features. Thus, IgG4 immunostaining is also an essential test for the diagnosis of IgG4-related disease1. In 2010, Cheuk and Chan6 proposed histological diagnostic criteria, including that the absolute number of IgG4-positive plasma cells in tissue should exceed 50 cells/HPF and the ratio of IgG4- to IgG-positive plasma cells should exceed 40% even though some people do not agree to this cutoff value of absolute IgG4-positive plasma cells in tissue1. An elevated serum IgG4 level (>135 mg/dL) is also helpful for diagnosis, but this test is not essential because its sensitivity and specificity are not sufficient. The serum IgG4 level is elevated in many non-IgG4-related diseases. Additionally, some patients with biopsy proven IgG4-related disease do not have elevated serum IgG4 level7. As noted earlier, to date, the clinical diagnostic criteria for IgG4-related disease have not been established. Therefore, more validity studies and comprehensive discussions with the professionals of various specialized fields and societies are needed to establish uniform and organ specific diagnostic criteria.
Although no randomized clinical trials for treatment of IgG4-related disease have been conducted, glucocorticoids are accepted as the first line treatment. Glucocorticoids appear to be effective in almost all patients with IgG4-related disease. However, in many cases, disease flares occur frequently. Immunosuppressants such as azathioprine, mycophenolate mofetil, and methotrexate are frequently used as steroidsparing agents or remission-maintaining drugs. Unfortunately, the patient in this case report did not respond well to the treatment with glucocorticoids. Recently, B-cell depletion with rituximab has been proven to be effective in recurrent or refractory diseases38. In 2012, Khosroshahi et al.8 published a report about successful treatment using B lymphocyte depletion therapy with rituximab, in 10 consecutive patients with steroid- and disease-modifying antirheumatic drugs-refractory IgG4-related disease. However, treatment with rituximab has a few problems. First, rituximab is known to develop potentially significant adverse effects. Infusion-related reaction and infection are the most common reported risks associated with B cell depletion. Second, the long-term effects of persistent B cell depletion are not clear. Therefore, more large prospective and long term follow-up studies are still needed to establish guidelines for use of rituximab in IgG4-related patients.
The one interesting finding in our case is the patient's age. The majority of patients are men (62% to 83%) and older than 50 years of age910. In 2008, Kamisawa and Okamoto5 described that the mean age of the patients was 66.5 years (range, 25-83 years). In our country, a case report of IgG4-related disease presenting as massive pleural effusion and thrombophlebitis had been published in 2014, in which the patient was also a middle aged man (48 years)11. It is important that the present case is the first case of extensive IgG4-related disease in a 16-year-old male patient in our country. Another interesting finding in our case is that the patient showed massive pleural effusion, especially chylothorax. IgG4-related disease can involve the pleura, and is sometimes associated with pleural effusion12. In 2014, Kato et al.13 reported a first case about IgG4-related pleuritis with chylothorax. In their report, the patient diagnosed of IgG4-related pleuritis by pleural biopsy and he showed right-sided chylothorax and left-sided non-chylothorax lymphocyte-predominant pleural effusion. The authors suggested that the right-sided chylothorax may be caused by rupture of the thoracic duct after resection of the lymph node. Or that it may be caused by compressed lymph nodes in the lymphatic channels and thoracic duct, impeding centripetal drainage of lymphatic flow13. The difference between previous case reports and our patient is that our patient showed bilateral chylothorax. Unfortunately, the triglyceride level in the pleural fluid before the VATS mediastinal biopsy was not checked. However, the patient showed bilateral pleural effusion before the VATS mediastinal biopsy. Therefore, we suggest that the bilateral chylothorax was one of the manifestations of IgG4-related disease, rather than operation related complication.
IgG4-related disease is an uncommon and recently recognized immune-mediated systemic condition that is increasingly reported. Because this disease can involve various organs, clinical manifestations may vary depending on the organs involved. We recommend that clinicians consider IgG4-related disease as a possible differential diagnosis in any age with a systemic or focal fibro-inflammatory condition, elevation of serum IgG4 level, and lymphoplasmacytic infiltration in pathology.
Notes
Conflicts of Interest: No potential conflict of Interest relevant to this article was reported.