Incidence and Risk Factors of Contrast-Induced Nephropathy after Bronchial Arteriography or Bronchial Artery Embolization
Article information
Abstract
Background
In uncontrolled hemoptysis patient, bronchial arteriography and bronchial artery embolization (BAE) is a important procedure in diagnosis and treatment. The aim of this study is to assess the incidence of contrast-induced nephropathy and the risk factors of contrast-induced nephropathy (CIN) after bronchial arteriography and BAE.
Methods
We retrospectively reviewed the medical records of the patients who underwent bronchial arteriography and BAE in two university hospitals from January 2003 to December 2011. CIN was defined as rise of serum creatinine more than 25% of baseline value or 0.5 mg/dL at between 48 hours and 96 hours after bronchial arteriography and BAE. We excluded patients who already had severe renal insufficiency (serum creatinine≥4.0) or had been receiving dialysis.
Results
Of the total 100 screened patients, 88 patients met the enrollment criteria. CIN developed in 7 patients (8.0%). The mean duration between the exposure and development of CIN was 2.35±0.81 days. By using multivariate analysis, serum albumin level was found to be significantly associated with the development of CIN (p=0.0219).
Conclusion
These findings suggest that the incidence of CIN was higher than expected and patients with hypoalbuminemia should be monitored more carefully to prevent the development of CIN after bronchial arteriography and BAE.
Introduction
Since Osborne et al. first used contrast media to get a picture of urinary tract in 1960s, the substance has been widely used for diagnosis and treatment1. As diagnostic and intervention methods increasingly employed contrast agents, the incidence of kidney diseases caused by the substance has risen. Contrast media is the third leading cause of iatrogenic acute renal failure occurred in hospital2. The incidence rate of contrast-induced nephropathy was estimated at 0.6% to 2.3%. However, the rate jumped to 20-30% in patients with chronic kidney disease3, diabetes, congestive heart failure and elderly people1,4-7.
Hemoptysis refers to the bleeding occurring in lung parenchyma8. The bronchial artery is the major source of bleeding in nearly 90% of cases9. Hemoptysis is an emergency condition. Patients with massive hemoptysis need urgent procedures such as bronchial artery embolization or lung lobectomy.
Effects of contrast media on kidney functions have been addressed in studies at home and abroad. But no study discussed the incidence and risk factors of kidney disorders as effects of contrast agent used for bronchial arteriography and embolization. Bronchial arteriography and embolization are urgently performed for patients with acute hemoptysis in emergency situation. And saline and N-acetylcysteine pretreatments are skipped in such an emergency situation. Based on this fact, an investigation into the association between the incidence and risk factors of kidney disorders and bronchial arteriography and embolization using contrast agents would provide useful information required to predict prognosis of patients. Authors retrospectively analyzed medical records of patients who underwent bronchial arteriography or bronchial artery embolization retrospectively. The aim of this study was to identify the incidence rate and risk factors of contrast-induced nephropathy.
Materials and Methods
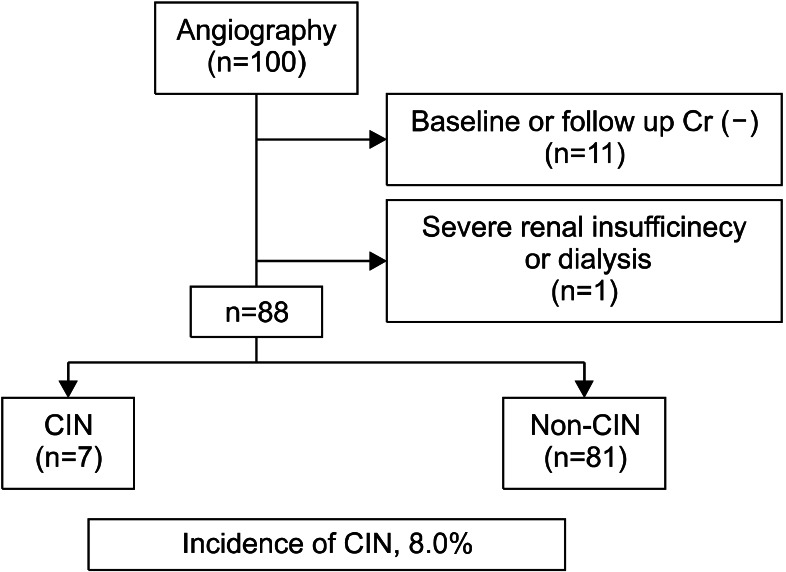
Medical records of patients who underwent bronchial arteriography or bronchial artery embolization at Hanyang University Hospital and Hanyang University Guri Hospital from January 2003 through December 2011 were analyzed retrospectively. Of patients who underwent either bronchial arteriography or bronchial artery embolization during the period, those who had no records for preopeative or postoperative creatinine level were excluded. Those had preoperative creatinine level of 4.0 mg/dL or higher and those who had undergone dialysis were also excluded. Among 100 concerned patients, 12 were excluded because of the above mentioned reasons. Medical records of 88 patients were reviewed for the present study.
Contrast-induced nephropathy is defined as a 0.5 mg/dL or higher (or a 25% or above) increase in creatinine between 48 and 96 hours after either bronchial arteriography or bronchial artery embolization from the baseline creatinine value10. Hypotension is defined by systolic blood pressure below 90 mm Hg or diastolic blood pressure below 60 mm Hg. Renal failure is defined as creatinine level exceeding the normal limit of 1.4 mg/dL used in the hospital.
As factors affecting contrast-induced nephropathy, age, sex, reuse of contrast agent in 3 days, test results (creatinine level, hematocrit and its change and serum albumin), bronchial artery embolization, dose of contrast agent, medications being taken, preopeative hypotension and concurrent illness were identified through review of the literature11,12. The association between each variable and contrast-induced nephropathy was investigated. Student-t tests or chi-square tests were performed for univariate analysis and multivariate logistic regression for bivariate analysis using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). p-values of less than 0.05 are considered significant. This study was approved by Clinical Trial Review Board of Hanyang University Hospital.
Results
1. Incidence rate of contrast-induced nephropathy
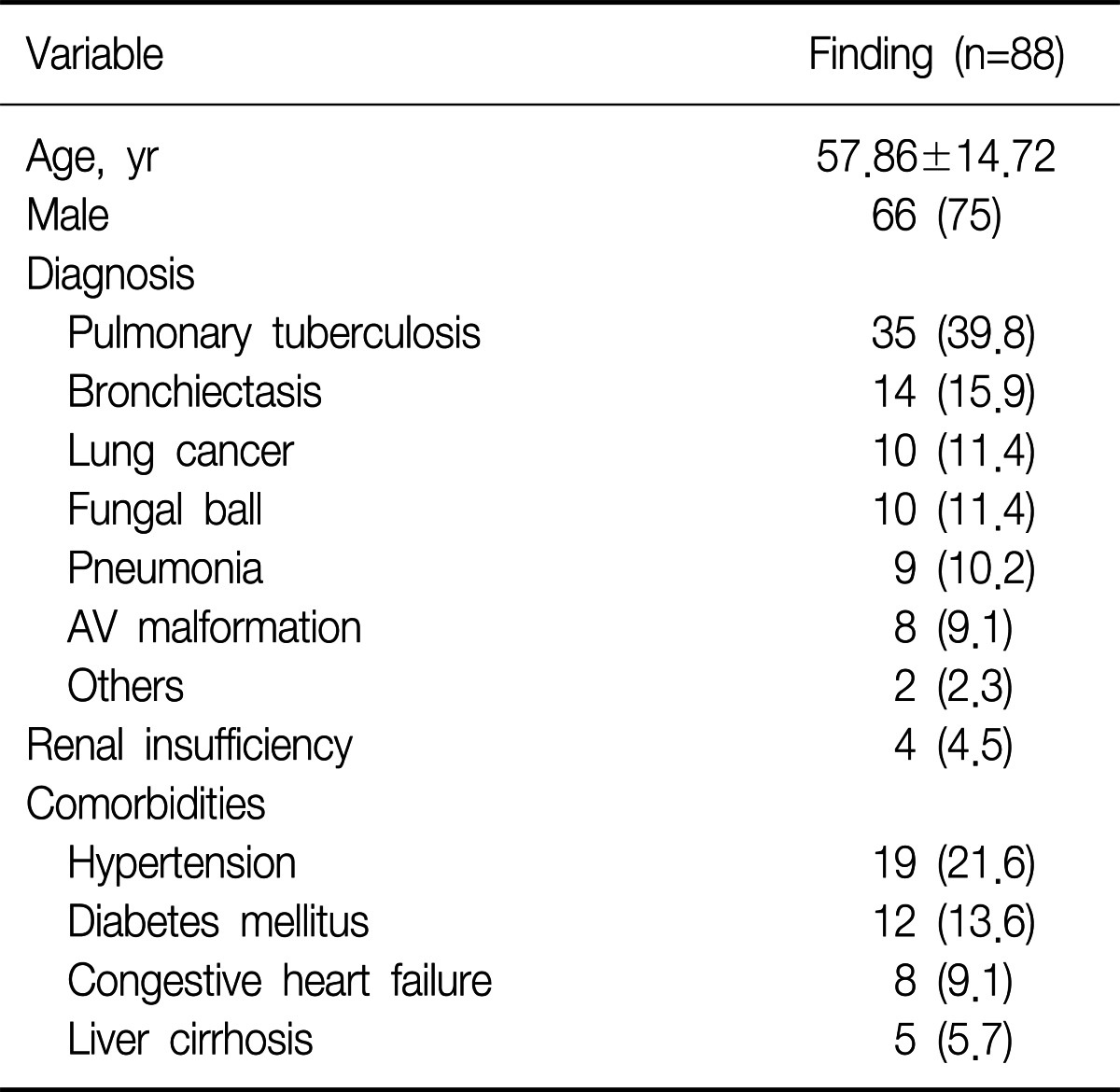
The average age of 88 patients was 57.8±14.72 years. Of 88 patients, 66 (75.0%) patients were men. Among admission diagnoses, tuberculosis was the most highest with 35 (39.8%) patients. Of those diagnosed as tuberculosis, 23 (65.7%) patients had active tuberculosis. Active tuberculosis was determined by computed tomography (CT) finding or positive sputum smear results or sputum incubation test results. Other concurrent illness included hypertension, diabetes, renal failure, and cirrhosis (Table 1). Of 88 patients, 7 (8.0%) patients developed contrast-induced nephropathy after bronchial arteriography or embolization (Figure 1). Visipaque (Iodixanol, 290 mOsm/kg) was used as contrast agent for 63 patients and ultravist (Iopromide, 770 mOsm/kg) for 25 patients.
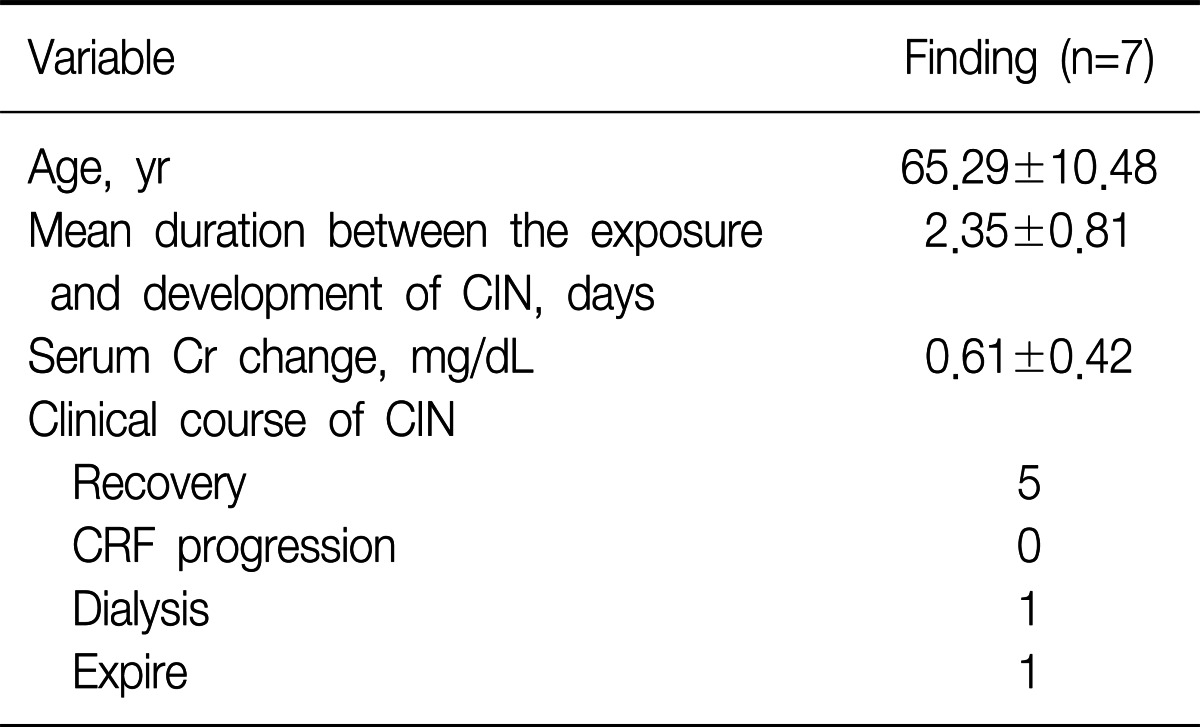
2. Clinical characteristics and progress
The mean age was 65.29±10.48 years in seven patients who developed contrast-induced nephropathy, which was confirmed mean 2.35 days after bronchial arteriography or embolization. An average creatinine change was 0.61 mg/dL. Of 7 patients with contrast-induced nephropathy, 5 recovered to the baseline creatinine level, one underwent dialysis and one died (Table 2).
3. Risk factors of contrast-induced nephropathy
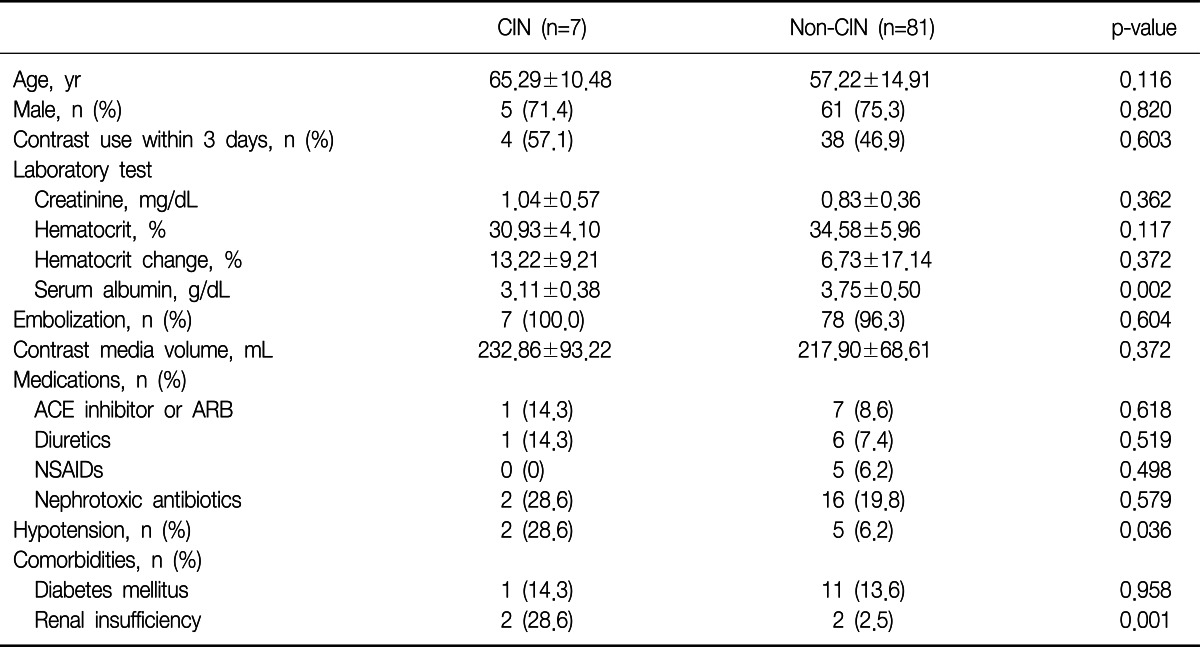
The mean age was 65.29±10.48 years and 57.22±14.91 years, respectively, in patients with contrast-induced nephropathy and patients without nephropathy. Creatinine level, hematocrit and hematocrit change and serum albumin were also compared for the two groups. Serum albumin was 3.11±0.38 g/dL and 3.75±0.50 g/dL, respectively, in the both groups. Univariate analysis (p=0.002) confirmed effects of low albumin on contrast-induced nephropathy. The entire group with contrast-induced nephropathy received bronchial artery embolization while 78 (96.3%) had the same procedure in the group without nephropathy. The dose of contrast agent was 242.86±93.22 mL and 217.90±68.61 mL, respectively, in the both groups. The difference was not significant between the groups (p=0.372). Contrast media dosage is known to be associated with the incidence of kidney disorders, according to earlier studies13.
Medications being taken included angiotensin-converting enzyme inhibitor or angiotensin receptor blocker (p=0.618), diuretic (p=0.519) and nonsteroidal antiinflammatory drug (p=0.498). However, no significant differences were observed between the two groups. Of 88 patients, 18 took nephrotoxic antibiotics, including aminoglycoside (n=16) and trimethoprim-sulfamethoxazole (n=2), before procedure. Effects of nephrotoxic antibiotics were not significant in the both groups (p=0.579). Hypotension was observed in two patients (28.6%) of the contrast-induced nephropathy group and five patients (6.2%) in the group without nephropathy. The difference was significant (p=0.036). Effects of renal failure were also significant between the two groups as 2 patients (28.6%) had renal failure in the group with nephropathy and 2 patients (2.5%) in the group without nephropathy (p=0.001) (Table 3).
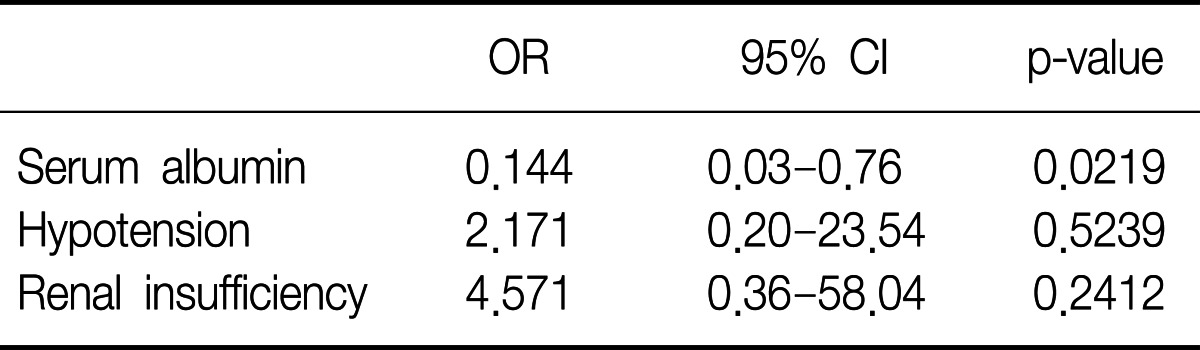
Among variables, low albumin, hypotension and renal failure showed significant differences between the two groups in univariate analysis. However, only low albumin was confirmed as a risk factor of contrast-induced nephropathy in multivariate logistic regression analysis (Table 4).
Discussion
In this study, the incidence rate of contrast-induced nephropathy was 8.0% after bronchial arteriography or embolization. The rate is much higher than the range of 0.6% to 2.3% found after CT scan3. Low albumin was identified as a risk factor of developing contrast-induced nephropathy in patients who underwent bronchial arteriography or embolization.
The use of contrast media is increasing in diagnostic and treatment practices thanks to evolving angiographic techniques. The incidence of contrast-induced nephropathy is growing as a result. Most studies were aimed to investigate effects of contrast media on kidney disease after coronary arteriography or CT scan. This is the first study investigating variables that affect contrast-induced nephropathy after bronchial arteriography and embolization.
Constrast-induced nephropathy is known to occur through two different mechanisms: atrophy of kidney vessels and cytotoxic effects of contrast media on the kidney. Renal blood flow is known to decrease by 30% to 45% within 2 to 4 hours after intravenous contrast media injection. As a result, kidney hypoxia is induced14,15. The second hypothesis claims that free radicals resulted from contrast agent injection induces cytotoxicity, which causes renal tubule damage16,17.
Serum albumin is the most abundant serum protein. It is responsible for 70% of the total osmotic pressure18. Although serum albumin exerts several functions in the body, its most important function is that it maintains the osmotic pressure in the vascular system. Also, it has antioxidant properties19. Some studies reported the preventive role of serum albumin for contrast-induced nephropathy through vascular expansion and antioxidant functions20. The mechanism involved in the association between nephropathy and low albumin is not clearly known. However, low albumin is likely responsible for the incidence of contrast-induced nephropathy by causing renal tubule cytotoxicity damage with free radicals.
It is found that contrast-induced nephropathy occurs within 1 to 2 days after exposure to contrast media. Contrast-induced nephropathy can be diagnosed with clinical symptoms such as oliguria and high serum creatinine level. Especially, serum creatinine level is an important indicator of contrast-induced nephropathy even when clinical symptoms such as oliguria do not show. It should be therefore checked within 1 to 2 days after the use of contrast media10,21.
The limitation of this study concerns of the sample size because this retrospective study used a limited number of subjects from the two university hospitals. Its results cannot be generalized to a larger population. However, the findings of this study would provide useful information for future multicenter, prospective studies aimed to investigate the prevalence rate and risk factors of contrast-induced nephropathy. Also low albumin identified as a risk factor of nephropathy underlines the need to alert for patients with low albumin before bronchial arteriography or embolization.