 |
 |
| Tuberc Respir Dis > Volume 86(1); 2023 > Article |
|
Sixty-two-year-old male presented with increasing cough, purulent sputum, and breathlessness for 3 days. Over the last 30 years, the patient has had a recurring cough with sputum, often interrupted by exacerbations, requiring multiple outpatient and emergency visits, and on several occasions, admissions for antibiotics, oxygen, and bronchodilator therapy. Clinical examination revealed tachypnoea with peripheral saturation of 91%, tachycardia, pallor, digital clubbing, with bilateral crackles, and wheeze on chest auscultation. Blood investigations and arterial blood gas analysis revealed anaemia and hypoxemia, respectively. Sputum microbiology, sweat chloride, and serum immunoglobulin profile were non-contributory. Chest radiograph showed bilateral lower zone cystic changes (yellow circles) with airspace opacities (white arrows) (Figure 1). A computed tomography scan of the chest revealed tracheomegaly (tracheal diameter 31.29 mm) with multiple tracheal and bronchial wall diverticula (red arrows), upper lobe emphysema (E), bilateral bronchiectasis (yellow arrows), and right lung consolidation (P) (Figure 2A, B). Flexible bronchoscopy confirmed multiple tracheal and bronchial wall diverticulosis (white arrows), with visible overlying atrophied longitudinal smooth muscle (black arrows), consistent with Mounier-Kuhn syndrome (Figure 2C). The bronchoalveolar lavage from the middle lobe grew Klebsiella pneumoniae. He was discharged after clinical and radiological results showed improvement following appropriate antibiotic, oxygen, and bronchodilator therapy. He continues having reasonable symptom control with regular home nebulized bronchodilator therapy and chest physiotherapy, and has completed vaccination for pneumococcus and influenza.
First described in 1932, Mounier-Kuhn syndrome is a rare clinical entity characterized by tracheobronchomegaly, which in turn leads to ineffective airway mucociliary clearance, recurrent lower respiratory tract infections, and bronchiectasis. Around 200 cases have been reported in medical literature, with less than twenty from the Indian subcontinent. Pathological examinations of the airways in these patients have demonstrated atrophy of the elastic and smooth muscle fibres. After this, there is a loss of the architectural framework of the central airways, leading to tracheobronchomegaly, outpouchings of the walls, and the development of blind diverticula. The diagnosis is often made on computed tomography scan of the chest, demonstrating a tracheal diameter above 30 mm (measured 2 cm above the aortic arch) and a right and left bronchial diameter of more than 20 and 18 mm, respectively. Flexible bronchoscopy, when performed, may aid in the diagnosis, by demonstrating airway secretions and central airway diverticulosis. Clinical management of these patients involves treatment of infective exacerbations with antibiotics and supportive therapies and long-term application of regular airway clearance techniques [1,2].
Notes
Fig. 1.
Chest radiograph postero-anterior view shows bilateral lower zone cystic changes (yellow circles) with air space opacities (white arrows).
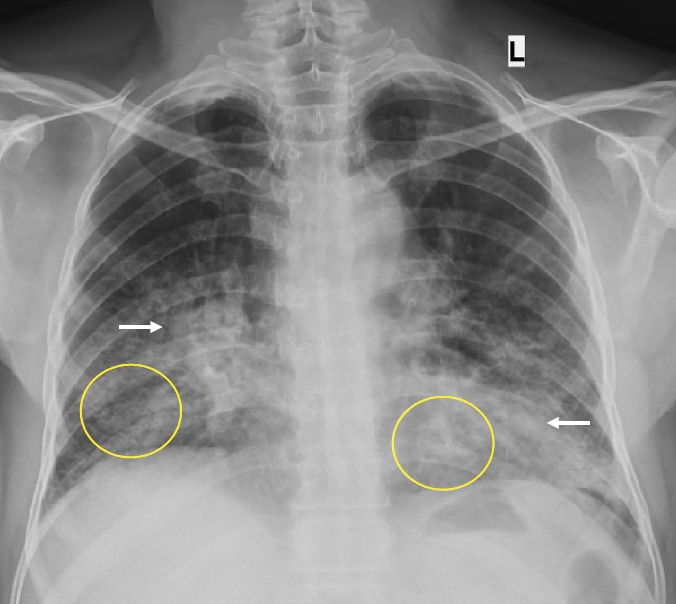
Fig. 2.
(A, B) Axial high-resolution computed tomography scan of the chest (A) at the level of the mid trachea 20 mm above the arch of aorta showing tracheomegaly with a measured transverse diameter of 31.29 mm, with bilateral paraseptal emphysema ‘E,’ and (B) at the level of carina showing bilateral bronchial dilatation, multiple bronchial diverticula (red arrows), bilateral upper lobe paraseptal emphysema ‘E’ and bronchiectasis (yellow arrows), and right upper lobe consolidation ‘P.’ (C) Flexible bronchoscopy showing lower trachea and carina, with diverticula over the posterior wall of the trachea, and medial wall of both main bronchus (white arrows), along with atrophy of the longitudinal smooth muscle seen over the posterior tracheal wall (black arrows).

-
METRICS

- ORCID iDs
-
Irfan Ismail Ayub

https://orcid.org/0000-0001-6109-0044 - Related articles


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



