1. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for prevention, diagnosis and management of COPD: 2023 report [Internet]. Fontana: GOLD; 2023 [cited 2024 Feb 16]. Available from:
http://goldcopd.org/2023-gold-report-2.
3. Stolz D, Mkorombindo T, Schumann DM, Agusti A, Ash SY, Bafadhel M, et al. Towards the elimination of chronic obstructive pulmonary disease: a Lancet Commission. Lancet 2022;400:921-72.


4. Yoo KH, Kim YS, Sheen SS, Park JH, Hwang YI, Kim SH, et al. Prevalence of chronic obstructive pulmonary disease in Korea: the fourth Korean National Health and Nutrition Examination Survey, 2008. Respirology 2011;16:659-65.


5. Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I, et al. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med 2022;10:447-58.



7. Sarkar C, Zhang B, Ni M, Kumari S, Bauermeister S, Gallacher J, et al. Environmental correlates of chronic obstructive pulmonary disease in 96 779 participants from the UK Biobank: a cross-sectional, observational study. Lancet Planet Health 2019;3:e478-90.


8. Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet 2022;399:2227-42.


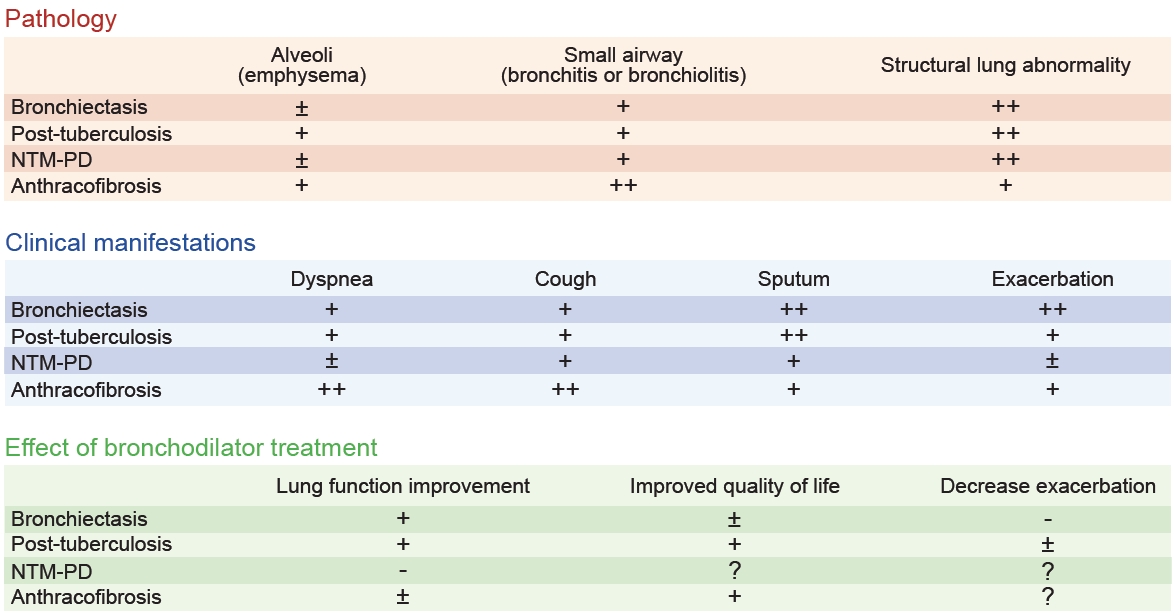
9. Lee H, Shin SH, Park HY, Lim SY. Can we call all obstructive lung diseases COPD? Eur Respir J 2023;61:2300462.


11. O’Donnell AE. Bronchiectasis: a clinical review. N Engl J Med 2022;387:533-45.


14. Hurst JR, Elborn JS, De Soyza A; BRONCH-UK Consortium. COPD-bronchiectasis overlap syndrome. Eur Respir J 2015;45:310-3.


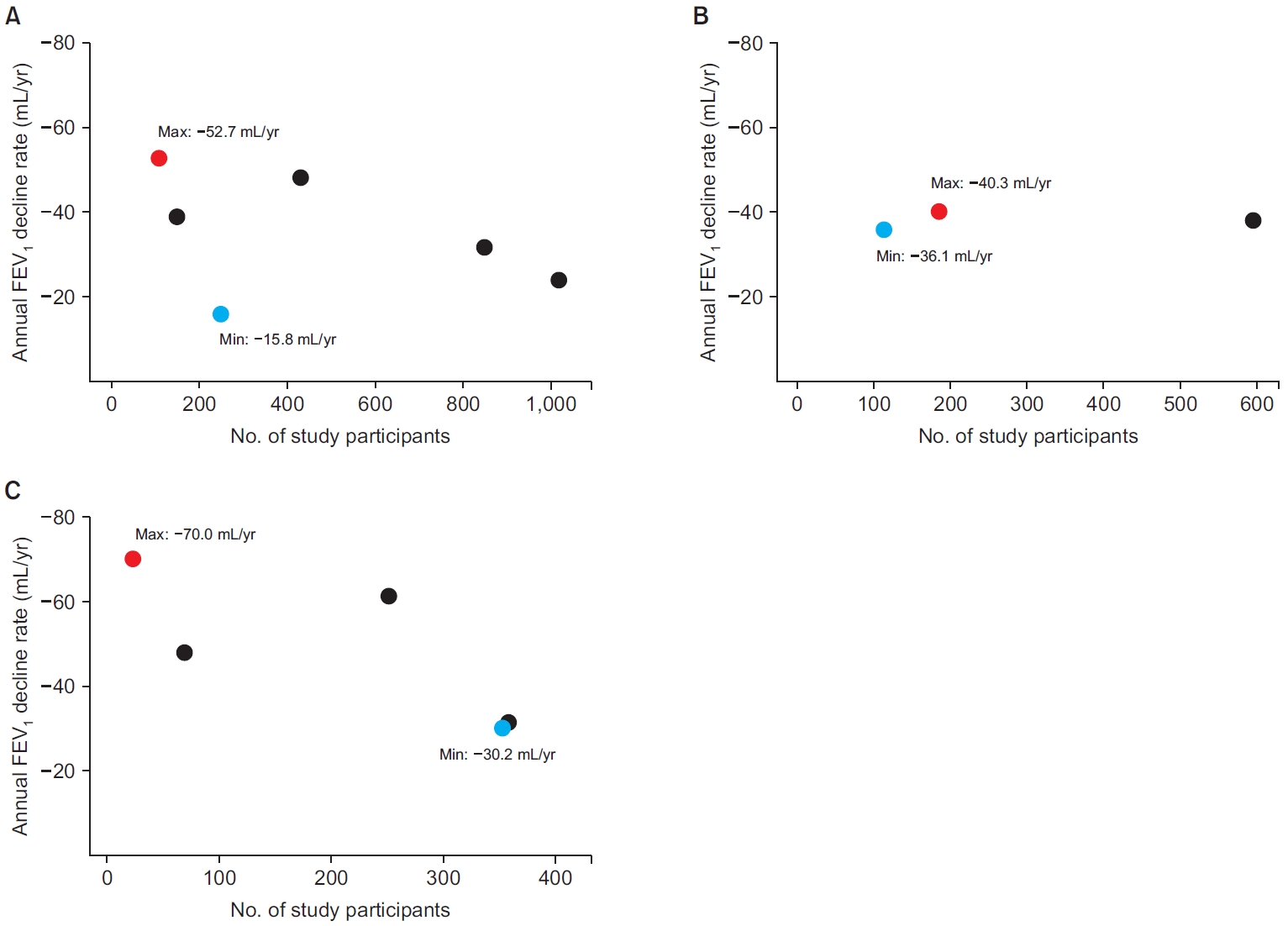
20. Borekci S, Gundogdu S, Harbiyeli DO, Musellim B. Annual FEV1 loss in patients with noncystic fibrosis bronchiectasis and affecting factors. South Med J 2022;115:328-32.


22. Dhar R, Singh S, Talwar D, Murali Mohan BV, Tripathi SK, Swarnakar R, et al. Clinical outcomes of bronchiectasis in India: data from the EMBARC/Respiratory Research Network of India registry. Eur Respir J 2023;61:2200611.


23. Kim NY, Lee CH, Jin KN, Lee HW, Heo EY, Kim DK, et al. Clinical deterioration and lung function change in patients with concomitant asthma and bronchiectasis. J Allergy Clin Immunol Pract 2022;10:2607-13.


24. Martinez-Garcia MA, Oscullo G, Posadas T, Zaldivar E, Villa C, Dobarganes Y, et al. Pseudomonas aeruginosa and lung function decline in patients with bronchiectasis. Clin Microbiol Infect 2021;27:428-34.

25. Martinez-Garcia MA, Soler-Cataluna JJ, Perpina-Tordera M, Roman-Sanchez P, Soriano J. Factors associated with lung function decline in adult patients with stable non-cystic fibrosis bronchiectasis. Chest 2007;132:1565-72.


26. Polverino E, Goeminne PC, McDonnell MJ, Aliberti S, Marshall SE, Loebinger MR, et al. European Respiratory Society guidelines for the management of adult bronchiectasis. Eur Respir J 2017;50:1700629.


30. Morton M, Wilson N, Homer TM, Simms L, Steel A, Maier R, et al. Dual bronchodilators in Bronchiectasis study (DIBS): protocol for a pragmatic, multicentre, placebo-controlled, three-arm, double-blinded, randomised controlled trial studying bronchodilators in preventing exacerbations of bronchiectasis. BMJ Open 2023;13:e071906.



31. Cazzola M, Martinez-Garcia MA, Matera MG. Bronchodilators in bronchiectasis: there is light but it is still too dim. Eur Respir J 2022;59:2103127.


37. Rhee CK, Yoo KH, Lee JH, Park MJ, Kim WJ, Park YB, et al. Clinical characteristics of patients with tuberculosis-destroyed lung. Int J Tuberc Lung Dis 2013;17:67-75.


45. Lam KB, Jiang CQ, Jordan RE, Miller MR, Zhang WS, Cheng KK, et al. Prior TB, smoking, and airflow obstruction: a cross-sectional analysis of the Guangzhou Biobank Cohort Study. Chest 2010;137:593-600.


46. Menezes AM, Hallal PC, Perez-Padilla R, Jardim JR, Muino A, Lopez MV, et al. Tuberculosis and airflow obstruction: evidence from the PLATINO study in Latin America. Eur Respir J 2007;30:1180-5.


48. Willcox PA, Ferguson AD. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir Med 1989;83:195-8.


49. Ross J, Ehrlich RI, Hnizdo E, White N, Churchyard GJ. Excess lung function decline in gold miners following pulmonary tuberculosis. Thorax 2010;65:1010-5.


50. Silva DR, Freitas AA, Guimaraes AR, D’Ambrosio L, Centis R, Munoz-Torrico M, et al. Post-tuberculosis lung disease: a comparison of Brazilian, Italian, and Mexican cohorts. J Bras Pneumol 2022;48:e20210515.


53. Allwood BW, Rigby J, Griffith-Richards S, Kanarek D, du Preez L, Mathot B, et al. Histologically confirmed tuberculosis-associated obstructive pulmonary disease. Int J Tuberc Lung Dis 2019;23:552-4.


58. Park HY, Jeong BH, Chon HR, Jeon K, Daley CL, Koh WJ. Lung function decline according to clinical course in nontuberculous mycobacterial lung disease. Chest 2016;150:1222-32.


66. Kim JH, Seo KW, Shin Y, Oh JS, Jun JB, Jeong J, et al. Risk factors for developing Mycobacterium kansasii lung disease: a case-control study in Korea. Medicine (Baltimore) 2019;98:e14281.


72. de Mello KG, Mello FC, Borga L, Rolla V, Duarte RS, Sampaio EP, et al. Clinical and therapeutic features of pulmonary nontuberculous mycobacterial disease, Brazil, 1993-2011. Emerg Infect Dis 2013;19:393-9.


73. Winthrop KL, McNelley E, Kendall B, Marshall-Olson A, Morris C, Cassidy M, et al. Pulmonary nontuberculous mycobacterial disease prevalence and clinical features: an emerging public health disease. Am J Respir Crit Care Med 2010;182:977-82.


75. Huang CT, Tsai YJ, Wu HD, Wang JY, Yu CJ, Lee LN, et al. Impact of non-tuberculous mycobacteria on pulmonary function decline in chronic obstructive pulmonary disease. Int J Tuberc Lung Dis 2012;16:539-45.


78. Park HJ, Kim JY, Kim HJ, Yim JJ, Kwak N. Lung function decline in non-tuberculous mycobacterial pulmonary disease according to disease severity. Int J Tuberc Lung Dis 2023;27:465-70.


79. Choi S, Potts KJ, Althoff MD, Jimenez G, Bai X, Calhoun KM, et al. Histopathologic analysis of surgically resected lungs of patients with non-tuberculous mycobacterial lung disease: a retrospective and hypothesis-generating study. Yale J Biol Med 2021;94:527-35.


80. Kubo K, Yamazaki Y, Masubuchi T, Takamizawa A, Yamamoto H, Koizumi T, et al. Pulmonary infection with Mycobacterium avium-intracellulare leads to air trapping distal to the small airways. Am J Respir Crit Care Med 1998;158:979-84.


82. Kurz SG, Zha BS, Herman DD, Holt MR, Daley CL, Ruminjo JK, et al. Summary for clinicians: 2020 clinical practice guideline summary for the treatment of nontuberculous mycobacterial pulmonary disease. Ann Am Thorac Soc 2020;17:1033-9.


85. Chung MP, Lee KS, Han J, Kim H, Rhee CH, Han YC, et al. Bronchial stenosis due to anthracofibrosis. Chest 1998;113:344-50.


86. Kim YJ, Jung CY, Shin HW, Lee BK. Biomass smoke induced bronchial anthracofibrosis: presenting features and clinical course. Respir Med 2009;103:757-65.


88. Jang SJ, Lee SY, Kim SC, Lee SY, Cho HS, Park KH, et al. Clinical and radiological characteristics of non-tuberculous bronchial anthracofibrosis. Tuberc Respir Dis 2007;63:139-44.

89. Jung SW, Kim YJ, Kim GH, Kim MS, Son HS, Kim JC, et al. Ventilatory dynamics according to bronchial stenosis in bronchial anthracofibrosis. Tuberc Respir Dis 2005;59:368-73.

90. Ucar EY, Araz O, Akgun M, Meral M, Saglam L, Kaynar H, et al. Bronchial anthracosis-anthracofibrosis: potential causes and clinical characteristics. Eurasian J Pulmonol 2014;16:17-20.

91. Amoli K. Anthracotic airways disease: report of 102 cases. Tanaffos 2009;8:14-22.
92. El Raouf BA, Kramer MR, Fruchter O. Bronchial anthracofibrosis: treatment using airway stents. Int J Tuberc Lung Dis 2013;17:1118-20.


93. Jamaati H, Sharifi A, Mirenayat MS, Mirsadraee M, Amoli K, Heidarnazhad H, et al. What do we know about anthracofibrosis?: a literature review. Tanaffos 2017;16:175-89.


94. Mirsadraee M, Ghaffari S, Saeedi P. Effect of salmeterol-fluticasone combination and tiotropium on clinical and physiological improvement of bronchial anthracofibrosis: a double blind randomized, cross over, placebo controlled, clinical trial. Tanaffos 2018;17:163-71.


97. Perlman DM, Maier LA. Occupational lung disease. Med Clin North Am 2019;103:535-48.










 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



