 |
 |
| Tuberc Respir Dis > Epub ahead of print |
|
Abstract
Notes
Authors’ Contributions
Conceptualization: Pham HQ, Pham KHT, Ha GH, Nguyen THT. Methodology: Pham HQ, Ha GH, Nguyen THT. Formal analysis: Pham HQ, Ha GH, Nguyen THT. Data curation: Pham TT, Nguyen HT. Writing - original draft preparation: Pham HQ, Ha GH, Nguyen THT. Writing - review and editing: Pham KHT, Oh JK. Approval of final manuscript: all authors.
Funding
This work was supported by the Domestic Master/PhD Scholarship Program of Vingroup Innovation Foundation.
One of the authors, Trang Huyen Thi Nguyen, received funding from the International Cooperation and Education Program (NCCRI·NCCI 52210-52211, 2023) of the National Cancer Center, Korea.
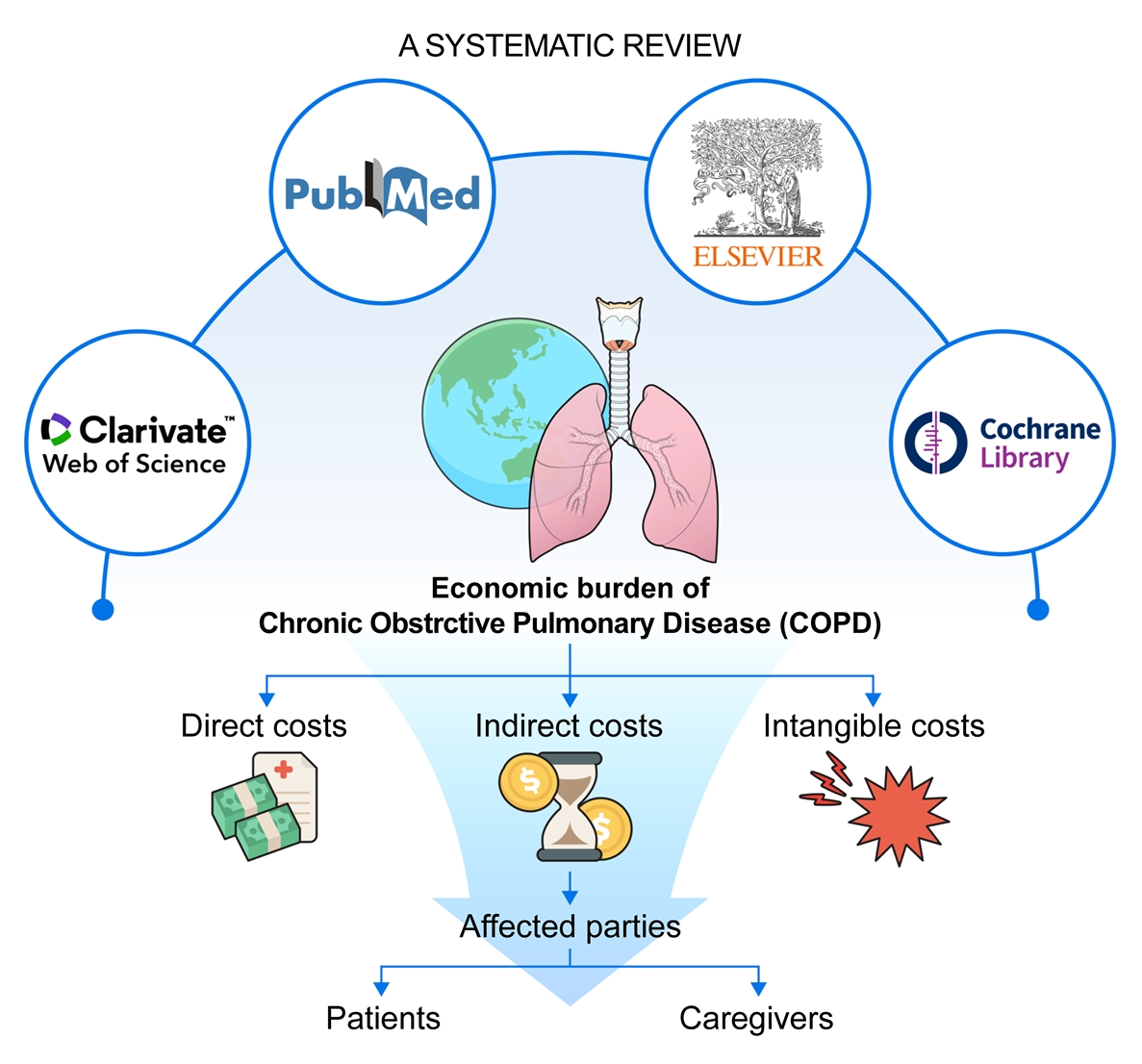
Fig. 1.

Table 1.
Table 2.
| No. | Main objective | Year | Country | Sample size | Study design | Perspective | Reference |
|---|---|---|---|---|---|---|---|
| 1 | Assess the cost-effectiveness of a home-based disease management intervention compared to usual management (U.M.) in individuals participating in the COPD Patient Management European Trial (COMET). | 2019 | France, Italy, Germany, Spain | 319 | Health economic evaluation study | Patients | [25] |
| 2 | Examine the overall healthcare costs linked to nebulized budesonide (nBUD) versus systemic corticosteroids (SCS) in patients experiencing acute exacerbations of COPD (AECOPD). | 2019 | China | 2,550 | Post hoc study | Patients | [26] |
| 3 | Systematically gather prospective outcome data from household members and demonstrate how these data can be integrated into a cost-utility analysis of a behavior change intervention for individuals with COPD. | 2019 | UK | 153 | Randomized controlledtrial | Patients/Caregivers | [27] |
| 4 | Comprehensively investigate the socioeconomic impact and resource utilization associated with COPD. | 2019 | Italy | NA | Retrospective study | Patients | [28] |
| 5 | Compare the utilization of healthcare resources at the end of life among three distinct groups of patients based on their "do not resuscitate" (DNR) directive status: those without a DNR directive, those with an early DNR (EDNR) directive established before entering the terminal hospitalization phase, and those with a late DNR (LDNR) directive established during the terminal hospitalization phase. | 2019 | China | 361 | Cross-sectional study | Patients | [29] |
| 6 | Evaluate both the direct and indirect costs associated with severe AECOPD within a tertiary care healthcare environment located in a high-prevalence region of North India. | 2019 | India | 129 | Cross-sectional study | Patients | [30] |
| 7 | Evaluate the economic burden of COPD in Greece. Additionally, the study aimed to identify and analyze potential determinants of the COPD economic burden. | 2019 | Greece | 351 | Cross-sectional study | Patients | [31] |
| 8 | The main objective of this study was to assess the long-term economic burden and benefits of implementing a regular program of systematic active case-finding for COPD in comparison to routine practice. | 2019 | UK | - | Cost-utility analysis | Patients | [32] |
| 9 | Investigate the association between clinically important deterioration(CID) in COPD and its impact on future economic and quality of life (QoL) outcomes. In addition, utilize a novel composite endpoint, CID, which evaluates the stability of the disease in COPD patients. | 2019 | USA | 3,769 | Post hoc study | Patients | [33] |
| 10 | Investigate and quantify the health-seeking costs associated with chronic cough, a distressing symptom often indicative of underlying health conditions like tuberculosis and chronic airways diseases, in the context of developing countries, with a particular focuson Malawi. | 2019 | Malawi | 608 | Economic study | Patients | [34] |
| Explore the coping mechanisms employed by individuals facing the financial burden of seeking care for chronic cough, such as borrowing money or selling household assets. | |||||||
| 11 | Describe the clinical and economic outcomes for patients with COPD based on their blood eosinophil (EOS) count. | 2019 | USA | 48,090 | Retrospective cohort study | Patients | [35] |
| 12 | Investigate healthcare resource utilization (HCRU) and related costs in patients COPD in a specialty care hospital setting in Finland | 2019 | Finland | 9,042 | Retrospective study | Patients | [36] |
| 13 | To explore and quantify the direct medical costs associated with COPD. | 2018 | Vietnam | 33,617 | Retrospective study | Patients | [37] |
| To identify and understand the main factors or variables that drive the costs of managing COPD. | [38] | ||||||
| 14 | To evaluate the consequences of applying the GOLD 2017 grading system to existing patients in the UK primary care. | 2018 | UK | 100 | Cohort study | Patients | [39] |
| To estimate the potential cost savings that could be achieved by implementing the treatment recommendations outlined in the GOLD 2017 guidelines for patients in the UK primary care. | 2018 | India | 24 | ||||
| 15 | The objective of this research was to investigate the economic impact, encompassing both direct and indirect costs, experienced COPD patients who were receiving treatment at selected tertiary care hospitals in South India. | 2018 | India | 24 | Cross-sectional study | Patients | [40] |
| 16 | To investigate how these costs COPD’s cost vary across different dimensions, including time, age, and disease stage. | 2018 | Sweden | 17,479 | Retrospective study | Patients | [41] |
| 17 | Assess how COPD, a condition associated with numerous comorbidities and substantial healthcare resource utilization, influences the social and economic aspects in Spain. | 2018 | Spain | 386 | Retrospective study | Patients/Caregiver | [5] |
| 18 | Measure the comprehensive burden of COPD by calculating both incremental direct and indirect costs associated with COPD. | 2018 | USA | 5,701 | Retrospective study | Patients | [42] |
| Assessing various aspects of cost, such as direct medical resource use, productivity metrics, and COPD-specific resource use and the associated expenses. | 2018 | Canada | 47 | ||||
| 19 | Conduct a cost-effectiveness analysis comparing the use of free O2 technology to manual oxygen-titration technology in the treatment s COPD patients who are hospitalized for acute exacerbations. | 2018 | Canada | 47 | Health economic evaluation study | Patients | [43] |
| 20 | Estimate the annual cost incurred by patients with COPD during the maintenance phase in Greece. | 2018 | Greece | 245 | Retrospective study | Patients | [43] |
| 21 | Determine the prevalence of COPD and cost of medical conditions treated on general internal medicine (GIM) inpatient services in seven hospital sites located in Toronto, Canada. | 2018 | Canada | 148,442 | Retrospective study | Patients | [44] |
| 22 | Investigate the hypothesis that incorporating total healthcare cost into the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index would improve the prediction of mortality in patients with COPD. | 2017 | Italy | 275 | Cross-sectional study | Patients | [45] |
| 23 | Assess and understand the clinical characteristics, treatment patterns, and the socioeconomic burden of COPD in Eastern Europe, with a specific focus on Bulgaria. | 2017 | Bulgaria | 426 | Cross-sectional study | Patients | [46] |
| 24 | Provide understanding of the cost-effectiveness of antibiotic prescriptions for COPD exacerbations and demonstrate the applicability of electronic health records (EHRs) in conducting such economic evaluations, particularly in the context of pragmatic RCTs. | 2017 | UK | 45,375 | Cohort study | Patients | [47] |
| 25 | Explore the economic burden of COPD in Greece. | 2017 | Greece | NA | Retrospective study | Patients | [12] |
| 26 | Evaluate the cost of treatment for patients with COPD in the context of Greece and assess the impact of the financial crisis on COPD patients. | 2017 | Greece | 189 | Cross-sectional study | Patients | [48] |
| 27 | Analyze the association between frequent comorbidities and common symptoms and the annual direct and indirect costs incurred by patients with COPD in Germany. | 2017 | Germany | 2,139 | Cohort study | Patients | [49] |
| 28 | Understand the disease burden associated with respiratory disorders, including allergic rhinitis (AR), asthma, COPD, and rhinosinusitis. | 2016 | South Korea | 999 | Cross-sectional study | Patients | [50] |
| 29 | Quantify and assess the total costs associated with COPD management in urban areas of China. | 2016 | China | 678 | Cross-sectional study | Patients | [51] |
| Explore and identify the factors that contribute to the high economic burden of COPD in these urban areas. | |||||||
| 30 | Quantify and analyze the annual cost of treating bronchiectasis (BE). in Spain, stratified by the severity of the disease as assessed by the FACED score. | 2016 | Spain | 456 | Cohort study | Patients | [52] |
| Identify and examine the specific parameters or factors that are associated with increased costs in the treatment of BE. | |||||||
| 31 | Evaluate and compare the cost-effectiveness of tiotropium (TIO) and glycopyrronium (GLY) in the management of COPD. | 2016 | Canada, Sweden, Spain, UK | NA | Cohort study | Patients | [53] |
| Consider the latest clinical evidence from the SPARK trial, which suggests that TIO is superior to GLY in reducing severe exacerbations. | |||||||
| 32 | Assess and report the prevalence and severity of respiratory symptoms in adults with a primary diagnosis of AR, asthma, COPD, and rhinosinusitis. | 2016 | Thailand | 1,000 | Cross-sectional study | Patients | [54] |
| Evaluate the impact of these respiratory diseases on work productivity, including work-related impairment and activity limitations experienced by affected individuals. | |||||||
| Analyze the economic burden associated with AR, asthma, COPD, and rhinosinusitis in terms of direct and indirect costs, including healthcare expenses and productivity losses. | |||||||
| 33 | Quantify and analyze the total economic burden of COPD in Italy. | 2015 | Italy | 275 | Retrospective study | Patients | [55] |
| 34 | Evaluate the economic implications of COPD in the period an official diagnosis. | 2014 | Denmark | 131,881 | Retrospective study | Patients | [56] |
| Analyze the economic consequences of COPD after diagnosis. | |||||||
| 35 | Provide an overview of the economic and management aspects of COPD in the United States. | 2013 | USA | Retrospective study | Patients | [57] | |
| 36 | Quantify and analyze the total costs associated with maintaining COPD therapy and managing acute exacerbations over a one-year timeframe. | 2012 | Canada | 285 | Retrospective study | Patients | [58] |
| 37 | Determine how the presence of anxiety and depression, as comorbidities, affect the utilization of healthcare resources and the associated costs among individuals with COPD. | 2011 | USA | 3,761 | Cohort study | Patients | [59] |
| 38 | Calculate and compare the annual COPD-related healthcare costs for each cohort, including both patient- and payer-paid costs. | 2010 | USA | 37,089 | Retrospective study | Patients | [60] |
| Determine the adjusted episode-level costs for various types of COPD-related visits, including outpatient, urgent outpatient, emergency department, standard admission, and intensive care unit stays. | |||||||
| 39 | Estimate healthcare resources utilization and costs of patients with COPD at the Italian pneumology departments | 2007 | Italy | 268 | Prospective study | Patients | [61] |
| Understand how the utilization of healthcare resources and costs vary among COPD patients at different stages of the disease. | |||||||
| 40 | Employing two different methods for cost estimation. The first method involved estimating the resources used and expenditures incurred by individuals with COPD that were directly attributable to the disease. | 2005 | USA | 8,300 | Retrospective study | Patient | [62] |
| Determining the average direct costs of COPD per patient, including a breakdown of costs associated with hospitalization and other healthcare utilization. | |||||||
| 41 | Investigate and assess the economic burden of COPD in seven countries: Canada, France, Italy, the Netherlands, Spain, the UK, and the United States. | 2003 | Canada, France, UK, USA, Spain, Netherlands, France | 3,265 | Economic analysis | Patient | [63] |
| 42 | Assess the direct medical costs associated with the provision of respiratory care for COPD patients on long-term oxygen therapy, taking into consideration both not-for-profit (NP) and profit-making (PM) health organizations responsible for home oxygen delivery. | 1996 | France | 234 | Retrospective study | Patient | [64] |
| 43 | Assess the cost-effectiveness of bronchodilators, theophylline (T) and ipratropium bromide (IB) therapies, taking into consideration their impact on the outcome of COPD, healthcare costs, and their known toxicity profiles. | 1993 | USA | 311 | Retrospective cohort study | Patient | [65] |
Table 3.
| Study | Country | Population/subpopulation | Total cost | Total medical cost | Pharmaceutical therapy | Outpatient cost | Total nonmedical cost |
|---|---|---|---|---|---|---|---|
| Dal Negro (2019) [28] | Italy | Patients with COPD | 3,988.09 (95% CI, 3,594.9-4,517.3) | 2,594.26 (95% CI, 1,316.6-4,043.3) | 678.15 (95% CI, 343.4-1,012.4) | 630.00 (95% CI, 282.2-977.8) | |
| Kourlaba et al. (2019) [31] | Greece | Patients with COPD | 3,223.05 (95% CI, 2,816.8-3,662.3) | 2,986.19 (95% CI, 260.8-3,368.5) | 1,163.30 (95% CI, 1,077.8-1,248.7) | ||
| Corsico et al. (2019) [66] | Italy | Patients with COPD | 3,600.19±6,391.0 | 1,549.16±1,668.7 | |||
| Fu et al. (2019) [29] | China | Patients with COPD | 7,685.23 | 7,685.23 | |||
| Koul et al. (2019) [30] | India | Patients with COPD | 1,404.38 | 258.71 | 108.49 | ||
| Lambe et al. (2019) [32] | UK | Patients with COPD | 1,098.29 | ||||
| Vo et al. (2018) [37] | Vietnam | Patients in Dong Nai Hospital | 70.07 | ||||
| Patients in Pham Ngoc Thanh Hospital | 1,291.55 | ||||||
| Lakiang et al. (2018) [39] | India | Patients with COPD | 1,131.99±534.8 | 514.42±324.1 | 52.08±6.3 | 331.82±99.5 | |
| Lisspers et al. (2018) [40] | Sweden | Patients with COPD | 12,921.30 | ||||
| Merino et al. (2018) [41] | Spain | Patients with COPD | 2,216.79±3,002.2 | 981.07±839.0 | 509.30±1,858.9 | 1,929.97±5,452.2 | |
| Poder et al. (2018) [42] | Canada | Patients with COPD | 13766.33 | ||||
| Verma et al. (2018) [44] | Canada | Patients with COPD | 10,180.53±15,842.7 | ||||
| Dzingina et al. (2017) [67] | Bulgaria | Patients with COPD | 3,096.70 | ||||
| Chen et al. (2016) [51] | China | Patients with COPD | 9,537.7±35,816.4 | 8,706.9±35,081.1 | 1,999.54±14,833.8 | ||
| Dal Negro et al. (2015) [55] | Italy | Patients with COPD | 2,679.95 (95% CI, 1,316.6-4,043.3) | 678.15 (95% CI, 343.4-1,012.9) | 630.00 (95% CI, 282.2-977.8) | ||
| Male COPD patients | 2,724.69 (95% CI, 2,053.2-3,396.2) | 667.27 (95% CI, 525.1-809.4) | 637.34 (95% CI, 462.7-810.6) | ||||
| Female COPD patients | 2,473.76 (95% CI, 1,462.4-2,507.0) | 688.48 (95% CI, 353.5-638.8) | 599.67 (95% CI, 403.7-795.7) | ||||
| Miller et al. (2005) [62] | USA | COPD patients | 2,507.00 | 375.00 |
Table 4.
| Study | Country | Population/subpopulation | Year | Indirect cost/Productivity loss | 95% CI |
|---|---|---|---|---|---|
| Dal Negro (2019) [28] | Italy | Patients with COPD | 2019 | 487.6 | 161.85-813.34 |
| Koul et al. (2019) [30] | India | Patients with COPD | 2019 | 94.8 | |
| Kourlaba et al. (2019) [31] | Greece | Patients with COPD | 2019 | 236.9 | 149.91-350.79 |
| Patients with COPD and CAT score ≤10 | 45.0 | 7.5-98.94 | |||
| Patients with COPD and CAT score >10 | 274.3 | 163.40-411.25 | |||
| Patients with mild level on Medical Research Council breathless scale | 199.4 | 80.95-370.28 | |||
| Patients with mild level on Medical Research Council breathless scale | 290.8 | 148.41-473.71 | |||
| Patients with mild level on Medical Research Council breathless scale | 269.8 | 92.94-454.22 | |||
| Patients with COPD at GOLD A | 33.0 | 0-76.45 | |||
| Patients with COPD at GOLD B | 97.4 | 47.97-157.40 | |||
| Patients with COPD at GOLD D | 398.8 | 223.36-613.13 | |||
| Merino et al. (2018) [41] | Spain | Patients with COPD | 2018 | 900.7 | 399.40-1,403.25 |
| Patel et al. (2018) [5] | USA | Patients with COPD | 2018 | 1,150.0 | |
| Souliotis et al. (2017) [12] | Greece | Patients with COPD | 2017 | 1,451.7 | |
| Nonpaid caregivers’ time | 1,207.8 | ||||
| Chen et al. (2016) [51] | China | Patients with COPD | 2016 | 3,265.3 | |
| Dal Negro et al. (2015) [55] | Italy | Patients with COPD | 2015 | 487.6 | 161.85-813.34 |
| Male COPD patient | 496.2 | 353.49-638.84 | |||
| Female COPD patient | 475.1 | 139.00-811.17 |
Table 5.
| Scale | Study | Population/subpopulation | Difference | SD | 95% CI |
|---|---|---|---|---|---|
| EQ-5D-5L score | Bhadhuri et al. (2019) [27] | Family members of patients on telephone coaching self-management | -0.029 | 0.14 | |
| Family members of patients on usual management | -0.019 | 0.10 | |||
| O'Reilly et al. (2007) [61] | Patients on admissions | -0.24 | 0.373 | -0.38 to -0.10 | |
| Happiness (scale 0 - 10) | Bhadhuri et al. (2019) [27] | Family members of patients on telephone coaching self-management | 0.22 | 1.41 | |
| Family member of patients with usual management | -0.11 | 1.24 | |||
| The COPD Assessment Test | Ladziak et al. (2019) [69] | Patients with triple-therapy inhaler combinations | -0.84 | -3.57 to 1.89 | |
| St George’s Respiratory Questionnaire for COPD | Bikmoradi et al. (2019) [72] | Patients with continuity of care model | 11.93 | ||
| Patients with routine care model | -1.15 | ||||
| Folch-Ayora et al. (2019) [82] | Male patients | -3.51 | |||
| Female patients | -2.24 | ||||
| Patients who had telephone education session | -6.83 | ||||
| Patient with usual management | -0.26 | ||||
| Caregiver burden questionnaire | Chu et al. (2019) [68] | Caregivers with <2 caregiving hours per day | 34.5 | 15.1 | |
| Caregivers with <3 caregiving hours per day | 45.8 | 10.5 | |||
| Caregivers with <5 caregiving hours per day | 59.8 | 5.1 | |||
| Caregivers with ≥6 caregiving hours per day | 67.4 | 6.3 | |||
| Caregivers of COPD patient | 57.3 | 14.6 |
References
-
METRICS

-
- 0 Crossref
- Scopus
- 525 View
- 37 Download
- ORCID iDs
-
Hai Quang Pham

https://orcid.org/0000-0003-4448-5436Kiet Huy Tuan Pham

https://orcid.org/0000-0002-6060-9868Trang Huyen Thi Nguyen

https://orcid.org/0000-0003-2954-4792 - Related articles
-
What Single Cell RNA Sequencing Has Taught Us about Chronic Obstructive Pulmonary Disease
Proposed Etiotypes for Chronic Obstructive Pulmonary Disease: Controversial Issues


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



